(NBC) - Andrew Felsted has been in an MRI machine more times than he can remember, but it's the past few that he's really looked forward to.
"He kind of thinks it's a little party to come and get an MRI now," says Missy Felsted, Andrew's mother.
That wasn't always the case. It used to be extremely tough for Andrew, and most children, to get an MRI. For starters, they have to stay still; sometimes for a couple of hours.
"Well, It's crucial. If they're moving, the MRI doesn't work," explains MRI technologist Ray Dushane.
Often, that meant having to sedate a child.
"There's a lot of complications that come along with sedating a child, especially for certain procedures," Missy says.
The most common problem was how sick the child felt after the medicine started wearing off.
"There would be hours for him to wake up, and then normally one or two days of throwing up because of the medications. So, an MRI was a three- or four-day procedure," Missy says.
That's on top of all the medication and procedures Andrew went through for brain cancer.
"He went through 30 days of radiation and 56 weeks of chemotherapy," says Erik Felsted, Andrew's father.
Recently the MRIs used to scan Andrew's brain actually became fun.
"It's really fun because you can just watch a movie and pretend you're not doing anything else," Andrew explains.
During his latest trip to the new Primary Children's Medical Center facility in Riverton, Utah Andrew showed reporters the goggles he wears during an MRI.
The "distraction" goggles show a movie, and Andrew can pick out any movie he wants. "It's nice," he says.
Even nicer for doctors, is how still he and other children stay during those long MRIs.
"Sometimes we finish the MRI early, and they're a little upset they can't finish their movie," Dushane says.
Andrew's parents are just happy that now a two-hour MRI doesn't mean two days of being sick.
"It really turned a long day at the hospital into a more positive experience," Erik says.
"It reduces all his anxiety coming here, which is really big," Missy says.
So big, Andrew says he can't wait for his next MRI. Doctors say Andrew has done well fighting his brain cancer. They expect him to live a full, normal life.
Wednesday, April 28, 2010
Teen walking, talking after traumatic crash
Their daughter was late getting home from work. The doorbell rang and on her way to answer the door, Alesha Gave saw the squad car in the driveway. “I knew it was bad,” Alesha said.
“It’s every parent’s worst dream,” her husband Dana added.
Their 19-year-old daughter Jordan had been in a car accident. That was all they knew as they made their way to St. Cloud Hospital. They didn’t know how badly she’d been hurt or if she was even alive.
Jordan was alive, but she had a broken pelvis, a broken left ankle, her lungs were collapsed and she had a brain injury.
Jordie, as her family calls her, had been on her way home from Family Dollar in Big Lake around 3:15 p.m. on Jan. 25. She took County Road 5 but doesn’t remember much beyond that.
It was dusk, snow was blowing and Jordan wasn’t familiar with the road.
According to her family, a vehicle was stopped at the intersection and Jordan swerved around it and ended up going through the stop sign, crashing into a vehicle that was on County Road 3.
“We’re assuming that she didn’t even see the other car that hit her,” Dana said.
The 2009 Milaca High School graduate was airlifted to St. Cloud Hospital where her family waited and wondered what would become of Jordan’s brain injury.
“I remember bits and pieces of the last week,” Jordan said of her three-week hospital stay. “But, nothing’s come back so far.”
Jordan didn’t speak at all that first week in ICU, primarily because she was in an induced coma. But doctors said she may never speak again.
“It was scary not knowing exactly how much of her we’d get back,” Alesha said.
Thankfully, today Jordan is walking and talking, but things have changed.
The teenager will need some more neurological testing to determine her learning ability.
She has some memory loss. For instance, her boyfriend, Derek Gregorich, and her watched a movie recently that they had seen before. But she has no recollection of having seen it.
“I tried to explain that she’d seen it before, but she couldn’t put it together,” Gregorich said.
“She’s had problems finding the words,” Alesha said of her daughter.
Even Jordan sees some of the changes in her, thanks to a journal she kept.
“I was a mean girl,” she said referring to the words she had written. “What was I thinking?”
After living in sweatpants and pajamas for the past three months, her first thought when she put her regular clothes on was, “Why is everything so tight?” Jordan’s dressing a little differently these days.
And she’s learned from others that she is more confident now and more comfortable with herself.
“She’s less moody,” her mother pointed out.
And there are some odd things, like the fact that she’s now afraid of bugs and she no longer enjoys chocolate.
“That’s when you know you’ve been hit on the head!” her dad jokes of a woman not liking chocolate.
But Mom says her daughter is definitely different than she was before the accident.
“She used to hide in her room,” Alesha said.
“She’s more outgoing,” Dana added.
“I’m not afraid to ask questions if I don’t understand something,” Jordan chimed in.
Jordan’s reaction time, cognitive thinking and problem solving skills are all worked on in occupational therapy.
“I don’t feel any different - brain-wise,” Jordan said.
The teen still likes to keep things clean and be organized.
“I haven’t seen you do the dishes yet,” Dana poked at his daughter. “Can you get that skill back?
One of the first foods the hospital staff gave Jordan was apple sauce.
“Yuck, that’s disgusting,” was her response.
“That’s when we knew she was still there,” Dana said. “There’s a big chunk of her that’s still her.”
While Jordan was in the hospital, she didn’t really understand why she was there. She’d tell people she had a broken ankle, which she could see, but would forget to mention the much more serious brain injury.
“She said it felt like it happened to someone else,” Alesha said. And though she had seen pictures of her Saturn, it wasn’t until she saw it in person that things really sank in for her.
Despite all the red tape with insurance, hospital bills and accident reports, the hardest part for Jordan’s parents is the “not knowing.”
“It could take up to a year for us to know where she’s at,” Alesha said.
Traumatic brain injury
With traumatic brain injuries (TBI), the injured can experience severe headaches, repeated vomiting or nausea, convulsions or seizures, an inability to awaken from sleep, dilation of one or both pupils of the eyes, slurred speech, weakness or numbness in the extremities, loss of coordination, and increased confusion, restlessness, or agitation.
Jordan seems to be one of the lucky ones and not only is she not angry about what’s happened to her, she’s kept a good sense of humor and a positive attitude, despite the mounting hospital bills for the girl who has no insurance.
“Physically, nothing’s hard,” Jordan, the petite teen, said of remembering how to walk. “But mentally, I take things harder than before.”
Yet, the only time she broke down, she said, was when the doctors told her she needs to take an IQ test.
A smart girl who graduated in the top 30, Jordan is concerned about the test, which she’ll have to take next month to determine if she has any permanent disability and if she’ll be able to attend college.
She also feels bad for what her parents have gone through and the financial difficulties for the family (Dana works at Woodcraft, Alesha is unemployed, and doctors won’t allow Jordan to return to work or drive yet).
“That’s okay, we’ve got you here,” Alesha reassured her daughter.
The tragic accident made everyone in the family realize how important family and friends are.
“Our family is closer than what I thought,” Dana, a former Foreston fire fighter, said. “We found out we have a lot of community support.”
That support will also come in the form of a benefit for Jordan on Saturday, May 8 at 5:30 p.m. at the Milaca Legion, which includes a spaghetti dinner, silent auction and bake sale.
Two days after the benefit, Jordan’s scheduled to have the remaining pieces of glass removed that are embedded in her lip and chin.
As for the Harry Potter-like scar on her forehead, she’s not sure if she’ll have plastic surgery or if she’ll keep it as a reminder.
Jordan’s aunt, Tracie Gave, sent Jordan a message on her CaringBridge site that said, “A very good friend of mine was in a bad car accident a few years ago and said she used to hate to have her picture taken-always worried about how her hair looked, or her clothes, or her weight. Now she says God gave her another chance to make those memories with her family so she’s in the pictures all the time!”
Jordan has two older sisters, Kim (26) and Amber (22). When the family gathers for Kim’s wedding later this year, it’s likely they’ll all be smiling in the photos - thankful that Jordan is with them.
“I’m alive and can only get better,” Jordan said.
“It’s every parent’s worst dream,” her husband Dana added.
Their 19-year-old daughter Jordan had been in a car accident. That was all they knew as they made their way to St. Cloud Hospital. They didn’t know how badly she’d been hurt or if she was even alive.
Jordan was alive, but she had a broken pelvis, a broken left ankle, her lungs were collapsed and she had a brain injury.
Jordie, as her family calls her, had been on her way home from Family Dollar in Big Lake around 3:15 p.m. on Jan. 25. She took County Road 5 but doesn’t remember much beyond that.
It was dusk, snow was blowing and Jordan wasn’t familiar with the road.
According to her family, a vehicle was stopped at the intersection and Jordan swerved around it and ended up going through the stop sign, crashing into a vehicle that was on County Road 3.
“We’re assuming that she didn’t even see the other car that hit her,” Dana said.
The 2009 Milaca High School graduate was airlifted to St. Cloud Hospital where her family waited and wondered what would become of Jordan’s brain injury.
“I remember bits and pieces of the last week,” Jordan said of her three-week hospital stay. “But, nothing’s come back so far.”
Jordan didn’t speak at all that first week in ICU, primarily because she was in an induced coma. But doctors said she may never speak again.
“It was scary not knowing exactly how much of her we’d get back,” Alesha said.
Thankfully, today Jordan is walking and talking, but things have changed.
The teenager will need some more neurological testing to determine her learning ability.
She has some memory loss. For instance, her boyfriend, Derek Gregorich, and her watched a movie recently that they had seen before. But she has no recollection of having seen it.
“I tried to explain that she’d seen it before, but she couldn’t put it together,” Gregorich said.
“She’s had problems finding the words,” Alesha said of her daughter.
Even Jordan sees some of the changes in her, thanks to a journal she kept.
“I was a mean girl,” she said referring to the words she had written. “What was I thinking?”
After living in sweatpants and pajamas for the past three months, her first thought when she put her regular clothes on was, “Why is everything so tight?” Jordan’s dressing a little differently these days.
And she’s learned from others that she is more confident now and more comfortable with herself.
“She’s less moody,” her mother pointed out.
And there are some odd things, like the fact that she’s now afraid of bugs and she no longer enjoys chocolate.
“That’s when you know you’ve been hit on the head!” her dad jokes of a woman not liking chocolate.
But Mom says her daughter is definitely different than she was before the accident.
“She used to hide in her room,” Alesha said.
“She’s more outgoing,” Dana added.
“I’m not afraid to ask questions if I don’t understand something,” Jordan chimed in.
Jordan’s reaction time, cognitive thinking and problem solving skills are all worked on in occupational therapy.
“I don’t feel any different - brain-wise,” Jordan said.
The teen still likes to keep things clean and be organized.
“I haven’t seen you do the dishes yet,” Dana poked at his daughter. “Can you get that skill back?
One of the first foods the hospital staff gave Jordan was apple sauce.
“Yuck, that’s disgusting,” was her response.
“That’s when we knew she was still there,” Dana said. “There’s a big chunk of her that’s still her.”
While Jordan was in the hospital, she didn’t really understand why she was there. She’d tell people she had a broken ankle, which she could see, but would forget to mention the much more serious brain injury.
“She said it felt like it happened to someone else,” Alesha said. And though she had seen pictures of her Saturn, it wasn’t until she saw it in person that things really sank in for her.
Despite all the red tape with insurance, hospital bills and accident reports, the hardest part for Jordan’s parents is the “not knowing.”
“It could take up to a year for us to know where she’s at,” Alesha said.
Traumatic brain injury
With traumatic brain injuries (TBI), the injured can experience severe headaches, repeated vomiting or nausea, convulsions or seizures, an inability to awaken from sleep, dilation of one or both pupils of the eyes, slurred speech, weakness or numbness in the extremities, loss of coordination, and increased confusion, restlessness, or agitation.
Jordan seems to be one of the lucky ones and not only is she not angry about what’s happened to her, she’s kept a good sense of humor and a positive attitude, despite the mounting hospital bills for the girl who has no insurance.
“Physically, nothing’s hard,” Jordan, the petite teen, said of remembering how to walk. “But mentally, I take things harder than before.”
Yet, the only time she broke down, she said, was when the doctors told her she needs to take an IQ test.
A smart girl who graduated in the top 30, Jordan is concerned about the test, which she’ll have to take next month to determine if she has any permanent disability and if she’ll be able to attend college.
She also feels bad for what her parents have gone through and the financial difficulties for the family (Dana works at Woodcraft, Alesha is unemployed, and doctors won’t allow Jordan to return to work or drive yet).
“That’s okay, we’ve got you here,” Alesha reassured her daughter.
The tragic accident made everyone in the family realize how important family and friends are.
“Our family is closer than what I thought,” Dana, a former Foreston fire fighter, said. “We found out we have a lot of community support.”
That support will also come in the form of a benefit for Jordan on Saturday, May 8 at 5:30 p.m. at the Milaca Legion, which includes a spaghetti dinner, silent auction and bake sale.
Two days after the benefit, Jordan’s scheduled to have the remaining pieces of glass removed that are embedded in her lip and chin.
As for the Harry Potter-like scar on her forehead, she’s not sure if she’ll have plastic surgery or if she’ll keep it as a reminder.
Jordan’s aunt, Tracie Gave, sent Jordan a message on her CaringBridge site that said, “A very good friend of mine was in a bad car accident a few years ago and said she used to hate to have her picture taken-always worried about how her hair looked, or her clothes, or her weight. Now she says God gave her another chance to make those memories with her family so she’s in the pictures all the time!”
Jordan has two older sisters, Kim (26) and Amber (22). When the family gathers for Kim’s wedding later this year, it’s likely they’ll all be smiling in the photos - thankful that Jordan is with them.
“I’m alive and can only get better,” Jordan said.
Testosterone directly amplifies but does not program male behaviors
New research uncovers some surprising information about how sex hormones control masculinization of the brain during development and drive gender related behaviors in adult males. The study, published by Cell Press in the April 29 issue of the journal Neuron, demonstrates that direct action of testosterone, the prototypical male hormone, is unnecessary for masculinizing the brain and behavior.
Testosterone and estrogen are thought to play an essential role in organizing and activating gender-specific patterns of behavior in sexually reproducing animals. Testosterone is produced by the testes and directly activates the androgen receptor (AR) in target tissues such as muscle. Estrogen is produced by the ovaries and is nearly undetectable in the circulation of males of most species. However, circulating testosterone in males can be converted into estrogen in the brain, and this testosterone-derived estrogen has been shown to control many male behaviors.
"It was known that testosterone and estrogen are essential for typical male behaviors in many vertebrate species," explains the study's senior author, Dr. Nirao M. Shah from the Department of Anatomy at the University of California, San Francisco. "However, how these two hormones interact to control masculinization of the brain and behavior remained to be established."
Dr. Shah and colleagues found that during the neonatal testosterone surge there is very little AR expressed in the developing brain, making it unlikely that testosterone signaling via AR plays a major role in masculinizing neural pathways. Importantly, they went on to show that the male pattern of AR expression in the brain was dependent on testosterone-derived estrogen signaling.
The researchers then used a genetic approach to knock out the AR in the mouse nervous system and observed that these mutants still exhibited male type mating, fighting, and territorial marking behaviors. However, these mutant males had striking reductions in specific components of these masculine behaviors. These results show that testosterone signaling via AR does not control masculine differentiation of the brain and behavior but regulates the frequency and extent of male typical behaviors.
"Our findings in conjunction with previous work suggest a model for the control of male pattern behaviors in which estrogen masculinizes the neural circuits for mating, fighting, and territory marking, and testosterone and estrogen signaling generate the male typical levels of these behaviors," concludes Dr. Shah. "It will be interesting in future studies to identify the molecular and circuit level mechanisms that are controlled by these hormones."
Testosterone and estrogen are thought to play an essential role in organizing and activating gender-specific patterns of behavior in sexually reproducing animals. Testosterone is produced by the testes and directly activates the androgen receptor (AR) in target tissues such as muscle. Estrogen is produced by the ovaries and is nearly undetectable in the circulation of males of most species. However, circulating testosterone in males can be converted into estrogen in the brain, and this testosterone-derived estrogen has been shown to control many male behaviors.
"It was known that testosterone and estrogen are essential for typical male behaviors in many vertebrate species," explains the study's senior author, Dr. Nirao M. Shah from the Department of Anatomy at the University of California, San Francisco. "However, how these two hormones interact to control masculinization of the brain and behavior remained to be established."
Dr. Shah and colleagues found that during the neonatal testosterone surge there is very little AR expressed in the developing brain, making it unlikely that testosterone signaling via AR plays a major role in masculinizing neural pathways. Importantly, they went on to show that the male pattern of AR expression in the brain was dependent on testosterone-derived estrogen signaling.
The researchers then used a genetic approach to knock out the AR in the mouse nervous system and observed that these mutants still exhibited male type mating, fighting, and territorial marking behaviors. However, these mutant males had striking reductions in specific components of these masculine behaviors. These results show that testosterone signaling via AR does not control masculine differentiation of the brain and behavior but regulates the frequency and extent of male typical behaviors.
"Our findings in conjunction with previous work suggest a model for the control of male pattern behaviors in which estrogen masculinizes the neural circuits for mating, fighting, and territory marking, and testosterone and estrogen signaling generate the male typical levels of these behaviors," concludes Dr. Shah. "It will be interesting in future studies to identify the molecular and circuit level mechanisms that are controlled by these hormones."
GAME: ConnecToo, a new line-drawing brain/finger teaser
We've just received a polite email from the maker of new Android game ConnecToo, who describes it as "sort of a drawing game". That was what he said in the informal email, at least - here's his more serious official description:
Certainly looks like a very polished product, and ConnecToo offers an original (as far as we know) take on the standard Android square-based puzzle game format. There's a free demo on the Android Market right now, while the paid-for version's listed as 69p in the UK if you like it.
It IS simple - you draw a line from one blue square to the next, then link up the yellows, then the other colours - but you can't cross the lines you make. Very straightforward, very nice. More screenshots and details can be found over on the developer's alarmingly personal site.
"ConnecToo is a game of logic, fast thinking and perception. Goal of game is to connect every two elements of same color. No problem, right? Well, the problem is, that lines you draw cannot cross each other, you are limited to grid and moreover you have time running fast"And if that description wasn't vivid enough for you, here's a few screenshots:
Certainly looks like a very polished product, and ConnecToo offers an original (as far as we know) take on the standard Android square-based puzzle game format. There's a free demo on the Android Market right now, while the paid-for version's listed as 69p in the UK if you like it.
It IS simple - you draw a line from one blue square to the next, then link up the yellows, then the other colours - but you can't cross the lines you make. Very straightforward, very nice. More screenshots and details can be found over on the developer's alarmingly personal site.
Mouse brain expression patterns of Spg7, Afg3l1, and Afg3l2 transcripts, encoding for the mitochondrial m-AAA protease
The m-AAA (ATPases Associated with a variety of cellular Activities) is an evolutionary conserved metalloprotease complex located in the internal mitochondrial membrane. In the mouse, it is a hetero-oligomer variably formed by the Spg7, Afg3l1, and Afg3l2 encoded proteins, or a homo-oligomer formed by either Afg3l1 or Afg3l2.
In humans, AFG3L2 and SPG7 genes are conserved, whereas AFG3L1 became a pseudogene. Both AFG3L2 and SPG7 are involved in a neurodegenerative disease, namely the autosomal dominant spinocerebellar ataxia SCA28 and a recessive form of spastic paraplegia, respectively.
Results: Using quantitative RT-PCR, we measured the expression levels of Spg7, Afg3l1, and Afg3l2 in the mouse brain.
In all regions Afg3l2 is the most abundant transcript, followed by Spg7, and Afg3l1, with a ratio of approximately 5:3:1 in whole-brain mRNA. Using in-situ hybridization, we showed that Spg7, Afg3l1 and Afg3l2 have a similar cellular pattern of expression, with high levels in mitral cells, Purkinje cells, deep cerebellar nuclei cells, neocortical and hippocampal pyramidal neurons, and brainstem motor neurons.
However, in some neuronal types, differences in the level of expression of these genes were present, suggesting distinct degrees of contribution of their proteins.
Conclusions: Neurons involved in SCA28 and hereditary spastic paraplegia display high levels of expression, but similar or even higher expression is also present in other types of neurons, not involved in these diseases, suggesting that the selective cell sensitivity should be attributed to other, still unknown, mechanisms.
Author: Tiziana SaccoEnrica BodaEriola HoxhaRiccardo PizzoClaudia CagnoliAlfredo BruscoFilippo Tempia
In humans, AFG3L2 and SPG7 genes are conserved, whereas AFG3L1 became a pseudogene. Both AFG3L2 and SPG7 are involved in a neurodegenerative disease, namely the autosomal dominant spinocerebellar ataxia SCA28 and a recessive form of spastic paraplegia, respectively.
Results: Using quantitative RT-PCR, we measured the expression levels of Spg7, Afg3l1, and Afg3l2 in the mouse brain.
In all regions Afg3l2 is the most abundant transcript, followed by Spg7, and Afg3l1, with a ratio of approximately 5:3:1 in whole-brain mRNA. Using in-situ hybridization, we showed that Spg7, Afg3l1 and Afg3l2 have a similar cellular pattern of expression, with high levels in mitral cells, Purkinje cells, deep cerebellar nuclei cells, neocortical and hippocampal pyramidal neurons, and brainstem motor neurons.
However, in some neuronal types, differences in the level of expression of these genes were present, suggesting distinct degrees of contribution of their proteins.
Conclusions: Neurons involved in SCA28 and hereditary spastic paraplegia display high levels of expression, but similar or even higher expression is also present in other types of neurons, not involved in these diseases, suggesting that the selective cell sensitivity should be attributed to other, still unknown, mechanisms.
Author: Tiziana SaccoEnrica BodaEriola HoxhaRiccardo PizzoClaudia CagnoliAlfredo BruscoFilippo Tempia
Stay brain sharp
Just because you are done with your education, doesn’t mean you need to stop learning. Keeping abreast of the latest happenings will help keep your mind agile and memory working well.
So many of us get so caught up in our jobs and daily chores that we don’t take time to read anything new or even try a new hobby. These can go a long way in keeping your mind young.
Become a frequent reader
Make it a point to read articles that may be differing with your point of view. This is a great way to challenge your brain and get yourself thinking. Be open to different people’s opinions. Read or listen, no matter how frustrated you may feel, as a bit of challenging knowledge is good.
Learn something new
This is a good thing to follow no matter your age. Pick something that interests or inspires you and follow it through. If you’ve always wanted to learn Salsa, join dancing classes. Have a guitar you bought but never use? Start taking guitar lessons. Playing an instrument also helps exercise some parts of the brain functioning especially while listening and reading written notes. By constantly adding to your repertoire of knowledge, you will be doing yourself a favour.
Teach someone
All of us are good at something or the other and teaching another can be beneficial. While teaching, your ‘student/s’ are bound to have many questions, which will prompt you to think and find out more. Surround yourself with people who ask smart questions and provide good insights as well.
Get some eye shut
Yes, sleeping for a good seven to eight hours daily is essential. Research shows that neural connections are made in the brain when you’re in your deepest phase of sleep.
Mind games
Games are not for kids! Solving a jigsaw puzzle, tackling a crossword game or even sudoku can do wonders for your brain. These will help your mind concentrate and work well. Further, they are a great way to de-stress and get a change from your regular work.
So many of us get so caught up in our jobs and daily chores that we don’t take time to read anything new or even try a new hobby. These can go a long way in keeping your mind young.
Become a frequent reader
Make it a point to read articles that may be differing with your point of view. This is a great way to challenge your brain and get yourself thinking. Be open to different people’s opinions. Read or listen, no matter how frustrated you may feel, as a bit of challenging knowledge is good.
Learn something new
This is a good thing to follow no matter your age. Pick something that interests or inspires you and follow it through. If you’ve always wanted to learn Salsa, join dancing classes. Have a guitar you bought but never use? Start taking guitar lessons. Playing an instrument also helps exercise some parts of the brain functioning especially while listening and reading written notes. By constantly adding to your repertoire of knowledge, you will be doing yourself a favour.
Teach someone
All of us are good at something or the other and teaching another can be beneficial. While teaching, your ‘student/s’ are bound to have many questions, which will prompt you to think and find out more. Surround yourself with people who ask smart questions and provide good insights as well.
Get some eye shut
Yes, sleeping for a good seven to eight hours daily is essential. Research shows that neural connections are made in the brain when you’re in your deepest phase of sleep.
Mind games
Games are not for kids! Solving a jigsaw puzzle, tackling a crossword game or even sudoku can do wonders for your brain. These will help your mind concentrate and work well. Further, they are a great way to de-stress and get a change from your regular work.
Genes Controlling Brain Wave Patterns Found
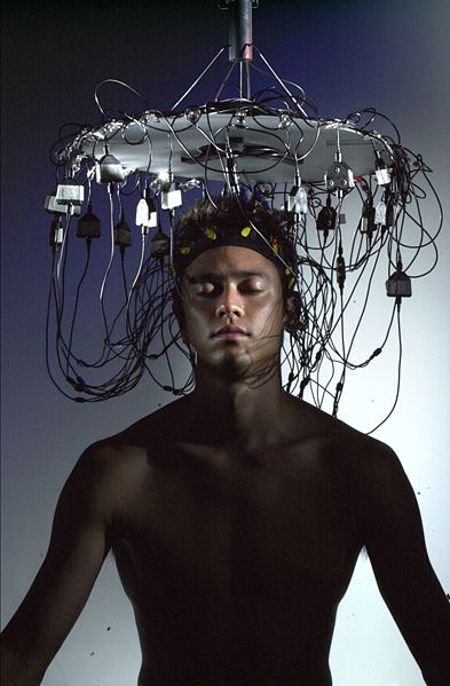 EEG machines were used in the new study to establish correlations between genes and brain wave patterns
EEG machines were used in the new study to establish correlations between genes and brain wave patternsIn a new scientific study, researchers detail the discovery of a new series of genes and associated pathways that appear to exert considerable influence on the brain wave patterns individuals' cortices exhibit. The new finding could be used as a surrogate marker, the team behind the study says, such as for instance in figuring out more complex genetic traits and diseases. They say that one of the genes found to be associated with the brain wave patterns has also been related with alcoholism in previous studies, PhysOrg reports.
“This important advance sustains our hope for the potential of genome-wide association techniques to further the study of complex genetic disorders such as alcoholism,” explains Kenneth R. Warren, PhD, who is the acting director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA). The organization is a division of the US National Institutes of Health (NIH). Details of the recent investigations appear in the latest issue of the esteemed publication Proceedings of the National Academy of Sciences (PNAS). The researchers used electroencephalography (EEG) to study the brains of participants, as each set of electrical wave patterns is unique to a single individual.
“One of the challenges in identifying the genes that underlie alcoholism is the large degree of genetic and environmental variability associated with the disease. Such variability has impeded even GWAS [genome-wide association studies] efforts to identify alcoholism genes. To overcome those difficulties, we used GWAS techniques to search for genetic variants related to EEG, or brain wave, patterns in a comparatively small sample of several hundred Native American individuals,” adds NIAAA Laboratory of Neurogenetics geneticist Colin A. Hodgkinson, PhD, who is also the first author of the PNAS paper. The study was carried entirely on Native Americans.
Of the genes found in the new study, one was found to be responsible for nearly 9 percent of all theta waves that the brain produces. Overall, two of the four most important frequencies were found to have their amplitude controlled by the genes the team identified. “While our main findings are for genes that influence EEG wave patterns, this study represents an important step toward the use of EEG as a surrogate marker for alcoholism. It also reveals new molecular pathways involved in addiction processes,” explains the chief of the NIAAA Laboratory of Neurogenetics, David Goldman, MD.
Exercise, Keep Your Brain Fit
As a trainer, I have always said that your life skills, focus and ability to improve various parts of your life can be positively affected by exercise. But, studies now support what many of us in the fitness industry have already seen firsthand. A recent study at the University of Pittsburgh School of Medicine found that middle aged monkeys who exercised on a treadmill had improved cognitive function than their sedentary counterparts. The study found that regular exercise’s positive impact on blood flow to the brain can help speed up the learning process. Prior studies out of Sweden have also showed that exercise, no matter what your age, can improve brain function.
While, I have especially seen seniors preserve much of their cognitive skills through exercise, there is now mounting evidence that kids, young adults and those in their middle age can boost brain power by implementing exercise into their daily life. Young to middle aged adults can truly benefit by the stress lowering effects of regular exercise as well as the documented ten percent brain boost. This is especially helpful during career building years. By lowering stress and anxiety, they’re less prone to become depressed, develop cardiovascular disease and diabetes. They’re also less prone to having a stroke which diminishes cognitive function and is the number one reason for rehabilitative care in the U.S.
Click here to comment on this article.
Studies show that exercise boosts blood flow to the brain and reduces the effects of aging on memory and brain function by promoting the growth of new nerve cells.
For the younger generations, there is a reason we hear the term student/athlete.
A study in the last several months focusing on teenage males found that those in the best cardiovascular strength out performed their less fit peers on various cognitive tests. The study also looked at the effect exercise had between the ages of 15 to18 for those who improved their fitness level. The results were positive not only physically, but academically as well as published in the Proceedings of the National Academy of The above study expands on prior findings that kids who participate in physical activity do better in school. Another study mentioned in a previous article of mine also focused on middle school kids. The study found that exercise not only benefits kid's health, but will benefit them in the classroom as well. That study,was released by the University of California in Los Angeles. The results showed that students who are physically fit did better on standardized tests than those who were less fit.
Joanne Sgro is a Television Fitness Expert, Certified Personal Trainer and Sport Nutritionist. She is Certified in Pilates, Pre-natal/Post-Partum, Yoga and Senior Fitness. She specializes in Weight Loss, Post-Rehab and Post Cancer Training. Joanne's fitness plans and recipes are available globally on her website www.fitnessanswer.com. She resides in the Phoenix, AZ area with her fiancé, where she runs her personal training business, Fitness Answer, LLC.
While, I have especially seen seniors preserve much of their cognitive skills through exercise, there is now mounting evidence that kids, young adults and those in their middle age can boost brain power by implementing exercise into their daily life. Young to middle aged adults can truly benefit by the stress lowering effects of regular exercise as well as the documented ten percent brain boost. This is especially helpful during career building years. By lowering stress and anxiety, they’re less prone to become depressed, develop cardiovascular disease and diabetes. They’re also less prone to having a stroke which diminishes cognitive function and is the number one reason for rehabilitative care in the U.S.
Click here to comment on this article.
Studies show that exercise boosts blood flow to the brain and reduces the effects of aging on memory and brain function by promoting the growth of new nerve cells.
For the younger generations, there is a reason we hear the term student/athlete.
A study in the last several months focusing on teenage males found that those in the best cardiovascular strength out performed their less fit peers on various cognitive tests. The study also looked at the effect exercise had between the ages of 15 to18 for those who improved their fitness level. The results were positive not only physically, but academically as well as published in the Proceedings of the National Academy of The above study expands on prior findings that kids who participate in physical activity do better in school. Another study mentioned in a previous article of mine also focused on middle school kids. The study found that exercise not only benefits kid's health, but will benefit them in the classroom as well. That study,was released by the University of California in Los Angeles. The results showed that students who are physically fit did better on standardized tests than those who were less fit.
Joanne Sgro is a Television Fitness Expert, Certified Personal Trainer and Sport Nutritionist. She is Certified in Pilates, Pre-natal/Post-Partum, Yoga and Senior Fitness. She specializes in Weight Loss, Post-Rehab and Post Cancer Training. Joanne's fitness plans and recipes are available globally on her website www.fitnessanswer.com. She resides in the Phoenix, AZ area with her fiancé, where she runs her personal training business, Fitness Answer, LLC.
The Brain Fires Differently in Reaction to Race
Different ethnicities elicit various responses
In a new study from researchers at the University of Toronto Scarborough, scientists reveal that the human brain fires differently when an individual sees another person from outside his or her own ethnic group or race. The investigation was meant to gage how the mirror-neuron-system functions when exposed to cues coming from people different from the test subjects. During the study, the participants were hooked up to electroencephalogram (EEG) machines, while they viewed videos showing short video clips of men and women from outside their race or ethnic group, ScienceDaily reports.Social neuroscientists have known for a long time that the brain must respond differently when exposed to such cues, and some have even proposed that this, in combination with other brain mechanisms, may offer some of the foundation for racism and discrimination. During the experiments, the participants, all of which were White, were asked to watch short video clips in which White, African American, South Asian and East Asian men picked up a glass of water, and then took a sip from it.
In previous researches, it was revealed that, when people look at others performing a task, a region of their brain called the motor cortex begins to fire in very much the same patterns as when they perform the actions themselves. But the new investigation reveals that this is only true when individuals relate to actions performed by people of the same race or ethnicity as their own. When participants looked at the video clips depicting minorities, their motor cortex exhibited a lot less activity than when they watched a White man doing the same thing.
In some instances, the level of activity was similar to when they were watching a blank screen. “Previous research shows people are less likely to feel connected to people outside their own ethnic groups, and we wanted to know why What we found is that there is a basic difference in the way peoples' brains react to those from other ethnic backgrounds. Observing someone of a different race produced significantly less motor-cortex activity than observing a person of one's own race. In other words, people were less likely to mentally simulate the actions of other-race than same-race people,” explains PhD student Jennifer Gutsell, the leader of the new research.
Psychopathy linked to brain damage
Psychopaths are known to be characterised by callousness, diminished capacity for remorse and lack of empathy.
However, the exact cause of these personality traits is an area of debate. The results of a new study show striking similarities between the mental impairments observed in psychopaths and those seen in patients with damage to the frontal lobes of the brain.
One previous explanation for psychopathic tendencies has been a reduced capacity to make inferences about the mental states of other people, an ability known as Theory of Mind (ToM).
On the other hand, psychopaths are also known to be extremely good manipulators and deceivers, which would imply that they have good skills in inferring the knowledge, needs, intentions, and beliefs of other people.
Therefore, it has been suggested recently that ToM is made up of different aspects: a cognitive part, which requires inferences about knowledge and beliefs, and another part which requires the understanding of emotions.
Simone Shamay-Tsoory, from the University of Haifa in Israel, along with colleagues from The Shalvata Mental Health Care Centre and the Rambam Medical Centre , tested the hypothesis that impairment in the emotional aspects of these abilities may account for psychopathic behaviour.
Earlier research from the same group had shown that patients with damage to the frontal lobes of the brain lack some of the emotional aspects of Theory of Mind, so they speculated that psychopathy may also be linked to frontal lobe dysfunction.
The emotional and cognitive aspects of Theory of Mind abilities were examined for participants in the new study, says a Haifa release.
Participants comprised different groups: criminal offenders, who had been diagnosed as having anti-social personality disorder with highly psychopathic tendencies, patients with damage to the frontal lobes of the brain, patients with damage to other areas of the brain, and healthy control subjects.
The pattern of impairments in the psychopathic participants showed a remarkable resemblance to those in the participants with frontal lobe damage.
However, the exact cause of these personality traits is an area of debate. The results of a new study show striking similarities between the mental impairments observed in psychopaths and those seen in patients with damage to the frontal lobes of the brain.
One previous explanation for psychopathic tendencies has been a reduced capacity to make inferences about the mental states of other people, an ability known as Theory of Mind (ToM).
On the other hand, psychopaths are also known to be extremely good manipulators and deceivers, which would imply that they have good skills in inferring the knowledge, needs, intentions, and beliefs of other people.
Therefore, it has been suggested recently that ToM is made up of different aspects: a cognitive part, which requires inferences about knowledge and beliefs, and another part which requires the understanding of emotions.
Simone Shamay-Tsoory, from the University of Haifa in Israel, along with colleagues from The Shalvata Mental Health Care Centre and the Rambam Medical Centre , tested the hypothesis that impairment in the emotional aspects of these abilities may account for psychopathic behaviour.
Earlier research from the same group had shown that patients with damage to the frontal lobes of the brain lack some of the emotional aspects of Theory of Mind, so they speculated that psychopathy may also be linked to frontal lobe dysfunction.
The emotional and cognitive aspects of Theory of Mind abilities were examined for participants in the new study, says a Haifa release.
Participants comprised different groups: criminal offenders, who had been diagnosed as having anti-social personality disorder with highly psychopathic tendencies, patients with damage to the frontal lobes of the brain, patients with damage to other areas of the brain, and healthy control subjects.
The pattern of impairments in the psychopathic participants showed a remarkable resemblance to those in the participants with frontal lobe damage.
When is Work Really Work?
One of the enduring artificial distinctions we make in our society is between real work and “work.” Physical labor is generally considered real work, and us desk jockeys are only doing “work,” which really shouldn’t be called work at all (so goes the belief) because it doesn’t involve physical exhaustion.
 Perceptions on this have changed somewhat over the years, but the underlying belief persists. It’s a noble gesture rooted in our past. This country was built on the backs of hardcore physical workers, and many believe that expanding the word “work” to include non-physical occupations dilutes its meaning. This thinking leads to statements like, “What Ted the construction worker does–now that’s work. It would be insulting to describe what I, an accountant, do as work compared to what he does.”
Perceptions on this have changed somewhat over the years, but the underlying belief persists. It’s a noble gesture rooted in our past. This country was built on the backs of hardcore physical workers, and many believe that expanding the word “work” to include non-physical occupations dilutes its meaning. This thinking leads to statements like, “What Ted the construction worker does–now that’s work. It would be insulting to describe what I, an accountant, do as work compared to what he does.”
The problem with this distinction, however noble, is that it’s patently false. For a long time, the act of thinking was considered a physically idle activity, presumably because one cannot see thinking taking place–but just the opposite is true. Thinking requires energy, and it derives this energy from the same source as physical labor: calories. The term “knowledge worker” made popular in the 80s by Peter Drucker and others is entirely accurate. Processing information to distill knowledge is energy intensive.
But what about the formula for work we all learned in physics? Work = Force x Distance. It still has a legitimate role, but it’s essentially a Newtonian tabulation that leaves out more than it includes. Can we measure the force and distance of thought? When the brain works through a complex problem, expending a great deal of energy to reach a conclusion, has it not overcome a distance through the force of mental exertion? I would argue yes, but the traditional formula is not equipped to quantify the brain’s activity.
What we know, however, is that the brain burns a lot of energy. Just to function, it consumes a calorie of energy every 3.5 minutes. The millions of neurons in your brain use 75% of the blood sugar from your liver, and 20% of the overall oxygen you take in every day. The more parts of the brain are exerted, the more glucose they pull from the bloodstream to convert into fuel for the production of neurotransmitters.
In his book, “Why Zebra’s Don’t Get Ulcers”, neurobiologist Robert Sapolsky references a study showing that chess masters, playing full days of chess during tournaments, burn 6000-7000 calories a day—similar to the level burned by Olympic athletes in training. That, of course, doesn’t mean that playing chess in general burns thousands of calories, but it does provide overall context for how much energy intense thought can require.
It should be said as well that none of this is justification for being sedentary. Physical activity provides many more benefits than simply burning calories. That aside, our definition of work needs a reboot, and it’s time we drop the artificial distinction between real work and “work.” Physical and mental work are variations on the same theme—and the brain has a major role to play in both.
 Perceptions on this have changed somewhat over the years, but the underlying belief persists. It’s a noble gesture rooted in our past. This country was built on the backs of hardcore physical workers, and many believe that expanding the word “work” to include non-physical occupations dilutes its meaning. This thinking leads to statements like, “What Ted the construction worker does–now that’s work. It would be insulting to describe what I, an accountant, do as work compared to what he does.”
Perceptions on this have changed somewhat over the years, but the underlying belief persists. It’s a noble gesture rooted in our past. This country was built on the backs of hardcore physical workers, and many believe that expanding the word “work” to include non-physical occupations dilutes its meaning. This thinking leads to statements like, “What Ted the construction worker does–now that’s work. It would be insulting to describe what I, an accountant, do as work compared to what he does.”The problem with this distinction, however noble, is that it’s patently false. For a long time, the act of thinking was considered a physically idle activity, presumably because one cannot see thinking taking place–but just the opposite is true. Thinking requires energy, and it derives this energy from the same source as physical labor: calories. The term “knowledge worker” made popular in the 80s by Peter Drucker and others is entirely accurate. Processing information to distill knowledge is energy intensive.
But what about the formula for work we all learned in physics? Work = Force x Distance. It still has a legitimate role, but it’s essentially a Newtonian tabulation that leaves out more than it includes. Can we measure the force and distance of thought? When the brain works through a complex problem, expending a great deal of energy to reach a conclusion, has it not overcome a distance through the force of mental exertion? I would argue yes, but the traditional formula is not equipped to quantify the brain’s activity.
What we know, however, is that the brain burns a lot of energy. Just to function, it consumes a calorie of energy every 3.5 minutes. The millions of neurons in your brain use 75% of the blood sugar from your liver, and 20% of the overall oxygen you take in every day. The more parts of the brain are exerted, the more glucose they pull from the bloodstream to convert into fuel for the production of neurotransmitters.
In his book, “Why Zebra’s Don’t Get Ulcers”, neurobiologist Robert Sapolsky references a study showing that chess masters, playing full days of chess during tournaments, burn 6000-7000 calories a day—similar to the level burned by Olympic athletes in training. That, of course, doesn’t mean that playing chess in general burns thousands of calories, but it does provide overall context for how much energy intense thought can require.
It should be said as well that none of this is justification for being sedentary. Physical activity provides many more benefits than simply burning calories. That aside, our definition of work needs a reboot, and it’s time we drop the artificial distinction between real work and “work.” Physical and mental work are variations on the same theme—and the brain has a major role to play in both.
MU Researcher Developing Test for Swallowing Disorder Treatments
COLUMBIA, Mo. – Muscle degeneration and confinement to a wheelchair are the hallmarks of Lou Gehrig’s disease, Parkinson’s, muscular dystrophy and other neurodegenerative diseases.
One of the silent, and most serious, symptoms of these diseases is losing the ability to swallow. Swallowing impairment, or dysphagia, affects about 500,000 people annually in the U.S., but little is known about the disorder and only a few temporary, behavioral treatments are available. Now, a University of Missouriswallowing disorders, leading to possible life-saving treatments. researcher is developing a test that might help pinpoint the neurological or physiological origins of
“A lot of these diseases attack the limbs, but you don’t die because your limbs don’t work,” said Teresa Lever, assistant professor in department of Communication Science and Disorders at the MU School of Health Professions. “Even though we can give patients feeding tubes with all the nutrients they need, there is no cure for swallowing disorders associated with neurodegenerative diseases, and patients still die early. I am trying to determine what is driving that mortality. If it is swallowing impairment, we need to know how the impairment starts and how we could treat it successfully, which would then improve patients’ lifespan and quality of life.”
Lever is trying to determine which components of the nervous system that control swallowing are impaired in patients with neurodegenerative diseases. To swallow, the brain must first sense the need to swallow, and then it must activate the right muscles to complete the process. In her study, she is developing an electrophysiological technique for use with mouse models of human neurological diseases that will show which regions of the brain are being used to swallow and which are short-circuiting. After finding which regions of the brain are not working correctly for each disease, treatments, such as stem cell therapy, gene therapy or certain medications, might be used to target those regions. The first disease that she is focusing on is Lou Gehrig’s disease, also known as amyotrophic lateral sclerosis or ALS.
“Instead of just treating a behavior, I am trying to determine the source of that behavior,” Lever said. “Swallowing is a reflex – you sense the need to swallow and then you have a muscular response. If we find that the sensory component of the swallowing reflex is being impaired along with the neuromuscular component, then many of these neurological diseases may be much more complex than we have been led to believe. It would tell us that our evaluation and treatment ofswallowing disorders should not just focus on the muscles and the nerves that stimulate them, but also on the sensory input. It would really create a paradigm shift in the research, especially for ALS which is classified as a motor neuron disease.”
Lever recently received a $300,000 grant from the National Institutes of Health for the study. She said that testing will begin in July and expects substantial results in the next two to three years.
One of the silent, and most serious, symptoms of these diseases is losing the ability to swallow. Swallowing impairment, or dysphagia, affects about 500,000 people annually in the U.S., but little is known about the disorder and only a few temporary, behavioral treatments are available. Now, a University of Missouriswallowing disorders, leading to possible life-saving treatments. researcher is developing a test that might help pinpoint the neurological or physiological origins of
“A lot of these diseases attack the limbs, but you don’t die because your limbs don’t work,” said Teresa Lever, assistant professor in department of Communication Science and Disorders at the MU School of Health Professions. “Even though we can give patients feeding tubes with all the nutrients they need, there is no cure for swallowing disorders associated with neurodegenerative diseases, and patients still die early. I am trying to determine what is driving that mortality. If it is swallowing impairment, we need to know how the impairment starts and how we could treat it successfully, which would then improve patients’ lifespan and quality of life.”
Lever is trying to determine which components of the nervous system that control swallowing are impaired in patients with neurodegenerative diseases. To swallow, the brain must first sense the need to swallow, and then it must activate the right muscles to complete the process. In her study, she is developing an electrophysiological technique for use with mouse models of human neurological diseases that will show which regions of the brain are being used to swallow and which are short-circuiting. After finding which regions of the brain are not working correctly for each disease, treatments, such as stem cell therapy, gene therapy or certain medications, might be used to target those regions. The first disease that she is focusing on is Lou Gehrig’s disease, also known as amyotrophic lateral sclerosis or ALS.
“Instead of just treating a behavior, I am trying to determine the source of that behavior,” Lever said. “Swallowing is a reflex – you sense the need to swallow and then you have a muscular response. If we find that the sensory component of the swallowing reflex is being impaired along with the neuromuscular component, then many of these neurological diseases may be much more complex than we have been led to believe. It would tell us that our evaluation and treatment ofswallowing disorders should not just focus on the muscles and the nerves that stimulate them, but also on the sensory input. It would really create a paradigm shift in the research, especially for ALS which is classified as a motor neuron disease.”
Lever recently received a $300,000 grant from the National Institutes of Health for the study. She said that testing will begin in July and expects substantial results in the next two to three years.
Growing more biotech technicians
I've heard for years that one of the things holding back Augusta's biotech industry growth is the lack of a technician workforce.
Augusta got a money splash to help address that: $400,000 for Work Ready certification.
The brain trust behind it is still trying to determine where exactly the money will go, said Lisa Palmer, interim vice president for economic development at Augusta Technical College. But it is creating a buzz among a team that's trying to get more biotech companies - and their jobs - in the Augusta region.
Augusta Tech already does a lot of Work Ready testing, but this money is supposed to help offset more of it.
It isn't just about breeding more people in lab coats, it is also about certifying the ones we've got.
So when the brain trust behind this latest push on biotech gets a prospect in town, there's numbers of ready-to-go workers to put on the table, not an anecdotal "we got you covered."
The budget for this $400,000 and the specific number of trained people is still being hammered out with the state, Palmer said.
"We're trying to advance bioscience, so we may use some money to buy equipment for a high school for their lab," she said. There are other examples they haven't gotten to yet.
The brain trust? Well, two of them are Julian Osbon, who has run a couple of medical companies in Augusta over the decades, and Annie Hunt Burriss, special assistant to the president of the Medical College of Georgia.
Osbon thinks the program will generate 10,000 Work Ready certificates by the time September 2011 rolls around. Consider that this is over a six-county area.
"If we're successful, we'll have biotech companies wanting to come to Augusta, not having to recruit them," he said.
There are some offshoots to the money. There is a desire to have a database filled with all these existing companies, many have only a handful of workers.
"You think you could go to the yellow pages and get all that, but it isn't that simple," Osbon said.
Knowing everyone helps establish collaboration of efforts.
Until then, there are more meetings planned to set budgets, create an industry group, host conferences. This is, after all, the first rung of the ladder.
AN EMAIL BLAST: Midtown Market has been sold to Mischelle Gutherie, the owner of Ready To Wear Again. No changes in operation are planned. First Thursday will go on each month.
BREAKING GROUND: SRP Federal Credit Union will turn the ceremonial dirt at 127 Davis Road on May 7.
The credit union is building a $2 million branch there. It is a relocation of the one that it in the nearby Kmart shopping center.
Remarks will begin at 11a.m. for anyone interesting in attending.
WHEN BUSINESS MEETS SPORTS: E-Z-Go's consumer-direct e-commerce site, shopezgo.com, will sponsor the No. 2 Chevrolet Silverado owned by Kevin Harvick Inc. in the NASCAR Camping World Truck Series O'Reilly Auto Parts 250 on Sunday.
The race will mark the second time this season that shopezgo.com has been the presenting sponsor of the truck.
Shopezgo.com is Augusta-based E-Z-Go's parts and accessories Internet sales place.
Augusta got a money splash to help address that: $400,000 for Work Ready certification.
The brain trust behind it is still trying to determine where exactly the money will go, said Lisa Palmer, interim vice president for economic development at Augusta Technical College. But it is creating a buzz among a team that's trying to get more biotech companies - and their jobs - in the Augusta region.
Augusta Tech already does a lot of Work Ready testing, but this money is supposed to help offset more of it.
It isn't just about breeding more people in lab coats, it is also about certifying the ones we've got.
So when the brain trust behind this latest push on biotech gets a prospect in town, there's numbers of ready-to-go workers to put on the table, not an anecdotal "we got you covered."
The budget for this $400,000 and the specific number of trained people is still being hammered out with the state, Palmer said.
"We're trying to advance bioscience, so we may use some money to buy equipment for a high school for their lab," she said. There are other examples they haven't gotten to yet.
The brain trust? Well, two of them are Julian Osbon, who has run a couple of medical companies in Augusta over the decades, and Annie Hunt Burriss, special assistant to the president of the Medical College of Georgia.
Osbon thinks the program will generate 10,000 Work Ready certificates by the time September 2011 rolls around. Consider that this is over a six-county area.
"If we're successful, we'll have biotech companies wanting to come to Augusta, not having to recruit them," he said.
There are some offshoots to the money. There is a desire to have a database filled with all these existing companies, many have only a handful of workers.
"You think you could go to the yellow pages and get all that, but it isn't that simple," Osbon said.
Knowing everyone helps establish collaboration of efforts.
Until then, there are more meetings planned to set budgets, create an industry group, host conferences. This is, after all, the first rung of the ladder.
AN EMAIL BLAST: Midtown Market has been sold to Mischelle Gutherie, the owner of Ready To Wear Again. No changes in operation are planned. First Thursday will go on each month.
BREAKING GROUND: SRP Federal Credit Union will turn the ceremonial dirt at 127 Davis Road on May 7.
The credit union is building a $2 million branch there. It is a relocation of the one that it in the nearby Kmart shopping center.
Remarks will begin at 11a.m. for anyone interesting in attending.
WHEN BUSINESS MEETS SPORTS: E-Z-Go's consumer-direct e-commerce site, shopezgo.com, will sponsor the No. 2 Chevrolet Silverado owned by Kevin Harvick Inc. in the NASCAR Camping World Truck Series O'Reilly Auto Parts 250 on Sunday.
The race will mark the second time this season that shopezgo.com has been the presenting sponsor of the truck.
Shopezgo.com is Augusta-based E-Z-Go's parts and accessories Internet sales place.
Medscape Great Debate: Radiologically Isolated Syndrome
 Mark Freedman, MD: Hello. I'm Dr. Mark Freedman, professor of neurology at the University of Ottawa in Ottawa, Ontario, Canada. I would like to welcome you to this Medscape Great Debate, entitled "Radiologically Isolated Syndrome: To Treat or Not to Treat." Joining with me are 2 other panelists, Dr. Bruce Cree, assistant professor of neurology at the University of California, San Francisco, and Dr. Fred Lublin, professor of neurology at the Mount Sinai School of Medicine in New York. Gentleman, radiologically isolated syndrome [RIS], is it MS and should we be treating it? Bruce?
Mark Freedman, MD: Hello. I'm Dr. Mark Freedman, professor of neurology at the University of Ottawa in Ottawa, Ontario, Canada. I would like to welcome you to this Medscape Great Debate, entitled "Radiologically Isolated Syndrome: To Treat or Not to Treat." Joining with me are 2 other panelists, Dr. Bruce Cree, assistant professor of neurology at the University of California, San Francisco, and Dr. Fred Lublin, professor of neurology at the Mount Sinai School of Medicine in New York. Gentleman, radiologically isolated syndrome [RIS], is it MS and should we be treating it? Bruce?I think the first thing we have to decide is what are we talking about -- what is radiologically isolated syndrome? I think the key point here is that we are talking about a patient who has had brain MRI [magnetic resonance imaging] done for some other reason and you see what looks like typical MS [multiple sclerosis] on the brain MRI -- periventricular plaques; contrast enhancement. And those are the cases that are defined as radiologically isolated syndrome. We are not talking about tiny little spots in the brain that you might see associated with migraine or age-related changes. These are patients who have had an imaging study done and who have a brain MRI that looks like MS, but no signs or symptoms, and no relapses that would tell you this is a clinically isolated syndrome [CIS]. So Dr. Lublin, would you treat or not treat a patient?
Dr. Freedman: Let me just interfere for a minute, because why would a patient [being seen] for a migraine get enhancement? Are we doing enhancing scans on patients who don't have curious neurologic symptoms? Is there not a suspicion that they might have something going on there and does that not make them more likely to have MS? Why would we be doing MRIs like that? What sort of patient populations are we talking about, because I see lots of people with that nonspecific stuff?
Fred Lublin, MD: There is no suspicion here. What we are talking about is people who had an MRI for some other reason completely unrelated to anything that could be construed as MS. Every once in a while you dig a little deeper and you may come up with something, but mostly we are talking about ones with a bad headache or pituitary abnormalities, workups for hormonal imbalances and things of that sort -- [even] a bump on the head. So if there is a suspicion there, that is not what we are talking about. We are talking about truly surprising findings on the MRI.
Dr. Freedman: But surely there are other things that can look exactly like MS. We have seen it repeatedly that there are many, many mimics of other diseases that show up with lesions identical to [those of] people with multiple sclerosis. How do you differentiate these?
Dr. Cree: I think there are relatively few things that look absolutely identical to MS. I have a pretty short list of things that I look for. Sarcoidosis is possible. I suppose CNS [central nervous system] lupus is possible, although that is pretty rare and I really don't see CNS lupus in my practice. Lyme disease can certainly present with lesions that look exactly like MS. [Also] other infectious etiologies, syphilis for example. So there are other things that can look like MS, but there is a way to go ahead and tease these things apart.
Dr. Freedman: So how would you do that? Before we could even consider treatment, I think we need to know what we are treating.
Dr. Cree: I think the point here is that these radiologically isolated syndromes look like MS, but we have no other causative etiology to explain the lesions on the brain MRI. I think the other point here, which is very interesting to me, is that it extends beyond the brain MRI and goes into the spinal cord. There was a study presented at this congress by Darin Okuda,[1] who showed that some of these patients who had brain MRIs also had some cervical spinal cord imaging. It was very interesting that of those patients who had cervical spinal cord imaging, a number of those patients also had lesions within the cervical cord. The key piece of data that he showed was that a majority of those patients -- 84% of the patients who had cervical cord lesion -- go on to develop the first attack of multiple sclerosis, the so-called clinically isolated syndrome. So the odds ratio of having a CIS or progression to primary-progressive MS [PPMS] -- because 2 of the patients ultimately went on to have PPMS -- was about 1 in 128, a very, very high odds ratio.
Dr. Lublin: This is with brain lesions?
Dr. Cree: This is with brain lesions as well.
Dr. Lublin: So they looked at the spine because the brain was abnormal?
Dr. Cree: The brain was abnormal and then the spine was looked at. So of those patients who had lesions in the cord, the odds ratio of going on and having a first attack is extremely high.
Dr. Freedman: So if this is the case Fred, why wouldn't you treat this?
Dr. Lublin: Well let's not get into treatment yet -- let's stick with "is this MS?" So I think that what Dr. Cree brings up in this study of Okuda's[1] is actually a very clever thing to do. Because of all of the mimics you mentioned -- and there are a few that have come up at this congress too -- one that is a mitochondrial disorder and a few others, the finding of lesions in the brain and the spinal cord significantly narrows the differential diagnosis and makes it much more likely to be MS. So for example when people get older [they may] get white dots in the brain, but you don't get white dots in the spinal cord. So I put increased weight on lesions in the spinal cord and I am not surprised at the result of them switching.
Whether it becomes MS or not -- when you call something MS -- gets into whether you want to talk about a clinical definition, a radiologic definition, which doesn't yet exist, or a biological definition. So we know that biologically people have MS who never ever have a clinical attack, and were it not for MRI scans we would never pick them up. The Danes did this study years ago with everybody getting autopsies and 1 in 1000 had the neuropathologic features of multiple sclerosis. When they went back into their centralized medical records, they couldn't find anything neurologic in those folks. So we know they exist. It's to the left of benign MS. Now because we have these scans and the MRI is so sensitive to picking up the lesions of MS, we are picking these folks up when they get a bump on the head or a bad headache or whatever. So biologically some of these people are MS.
But then you have to say when are you willing to tell them that it is MS? Does it matter if they never would have had another clinical event ever?
Dr. Cree: But Fred, this gets right into the issue of CIS as well. So we know from longitudinal studies that patients who have a single attack and an abnormal brain MRI have a great likelihood of having further events. But not everybody. There are about 10% of patients who don't have another event over the next 14 years if you believe the Queen Square data.[2] So the vast majority do have another event and based on that we often wind up recommending treatment for those patients.
The newest set of [MS] diagnostic criteria that have been proposed, the MAGNIMS [Magnetic Resonance Imaging in MS] criteria,[3] [include] patients who have an abnormal brain MRI with evidence of dissemination in time by a contrast-enhanced lesion as well as other lesions that do not enhance with contrast, along with some other criteria for dissemination in space. [These criteria] are actually just as good as the McDonald criteria or the International Panel criteria from 2001 and 2005, where you show dissemination in time by serial MRI imaging. So I know you have sat on both of those panels and presumably are going to be reviewing the MAGNIMS criteria. Aren't you convinced that in the case of CIS with an abnormal MRI that meets MAGNIMS criteria that this is the same thing as MS?
Dr. Lublin: So CIS is not the issue here yet. I mean we are again moving to the left. You have established MS, clinically isolated syndrome, and here to the left you have radiologically isolated syndrome. Then you have all the people who have MS who we will never find out about because they never come to clinical or radiological attention. The CIS story is very compelling, and it is even more compelling than you laid out in the sense that all you need is 2 lesions. So the Queen Square data[2] [suggest that] if you have 1 lesion, [you have an] 80% chance in 14 years of converting to definite MS or having another attack. All of the clinical trials starting with CHAMPS [Controlled High-risk Avonex Multiple Sclerosis][4] and moving forward took 2 MS-looking lesions; MS as judged by people who know how to read MRI scans and pick out what looks like an MS lesion. They all showed highly significant benefit. It took us awhile and we still haven't convinced everyone that those folks ought to be treated. But back in 1993 when we came out with the first treatment for relapsing MS it took us a while to convince people that they ought to treat for that -- we moved past that. CIS I think most people treat -- [although] there are still debates and there are areas around the world where you can't get treated -- but that is based on well-established criteria and clinical trials.
For RIS we don't have that information. We do have a few studies now: we have LeBrun,[5] we have Okuda.[1] LeBrun did a follow-up,[6] and the conversion rate of those people ranged from 25% to 30% over 5 years clinically and higher, maybe double that, radiologically. But we don't know what the impact is of treating at that stage. You can by extension say, well why not? It is not unreasonable, which is why we could have flipped a coin as to how to sort out which side we were going to be on. I don't think it is necessarily unreasonable, but you have to recognize that as difficult as it is to say [to a patient] with CIS "we are going to treat you for something that I can't diagnose yet, but I know you will do better this way," [with RIS] you are talking about at least another exponential change: "you don't really have clinical MS and you have never had an attack, but we want you to take one of these therapies, which at best is going to be annoying -- and by the way I don't know when to stop it and you are now at risk for MS so you have to think about that, too." It is just tough.
I don't think there is a knee-jerk answer to this. I think that a changing MRI would bother me. I think it probably bothers you and I think that is what your colleague is showing, but I am not sure whether all of these people ought to be treated or if it will do any good. Saying that, I recognize that it's our work and the work of others [to recognize] that every exacerbation potentially counts, with 50% of individuals having something residual.
Dr. Cree: Every cubic millimeter of brain tissue that is acutely demyelinating has about 10,000 axons being transected based on Bruce Trapp's work, and once those axons are transected, they don't grow back. Once they die, the neurons die and I think that although we are still waiting for proof that neurodegeneration is caused by neuroinflammation, I am pretty swayed by these data and really think that is the key issue at stake here. If we go ahead and imagine a scenario where we have a treatment trial in RIS and we stratify that treatment trial where we are just looking at the patients who have spinal cord lesions and we find that we are able, with anti-inflammatory therapies, to delay the time significantly until the first actual clinical event, then we have done our patients a service. So from the extension of knowing what we know about MS, knowing what we know from the MAGNIMS study,[3] knowing what we know by putting up all of these MRI scans over the years and seeing more lesions than the patient presented with. Say a patient comes in with optic neuritis and the brain is chalk full of lesions; we know those lesions showed up at some point beforehand. Doesn't it make sense to actually consider treatment in such a patient?
Dr. Lublin: It makes sense, but you would want to have evidence.
Dr. Cree: Absolutely.
Dr. Lublin: The Bruce Trapp information is interesting. What is not clear to me is whether that is the case with every patient. What he is showing are the patients who came to his biopsy table [and there was] evidence of axonal degradation in some of them. One of the challenges that we now have is to phenotype people as to whether they are demyelinators or axon degenerators or both, and I don't know the answer to that. The pathologists haven't been able to answer the question for me either. They are interested in looking at a number of different things, but no one has answered the simple question as to whether someone is more degenerative or more inflammatory or demyelinated. We know there are people who have bad demyelination who get a fever, [become] septic and go from walking to plegic. You hydrate them and you treat their fever and they are back to walking again. Well they can't be degenerators. They have to be demyelinators. So there is a difference there, and I think these are the kinds of things we need to sort out. What we need to convince people is evidence. The other thing we need to deal with is what is the threshold under which you can put out a general recommendation to the neurologic community to treat, because it is a little different when your colleagues are looking at these scans and making decisions and when we put it out as a general recommendation for everybody.
Dr. Cree: Sure, of course. I would agree entirely at this point. I don't think we can make general recommendations. I think even in the subgroup of patients who really look like they probably have MS, we still don't know for sure whether treatment should be done or not, but I certainly would consider it. I have in my personal practice only treated one RIS patient and that patient had contrast-enhancing lesions and I also found evidence of subtle asymmetry on her neurological examination. I discussed treatment with her and she ultimately went on to treatment and ultimately went on to have CIS despite treatment and ultimately went on to have RRMS [relapsing-remitting MS] despite treatment. We now finally have her stabilized. It is a very interesting dilemma about what to do when you are faced with a real-life patient who is high functioning, who is active at work, young, and wants everything done for them. The question is, what do you do?
Dr. Freedman: If we had a treatment that was a simple pill with virtually no side effects and a long safety record, would you hesitate?
Dr. Lublin (to Dr. Cree): Did you make that decision on one scan or a follow-up?
Dr. Cree: She actually came in with a single scan and on the scan she would have met MAGNIMS criteria with a couple of contrast-enhancing lesions and other lesions that were T2 bright and a couple of T1 dark, again suggesting that some of the lesions had a more chronic nature. On the exam there were some very subtle findings that were there, but I was able to convince myself and we entered into a discussion and she ultimately decided to move forward with therapy.
Dr. Lublin: So I would disagree with that. I have treated some as well, but I always look for change over time. I want to see the enhancing lesions get better in the sense of not enhancing and I want to see something new. It doesn't matter if it is gad[olinium-enhancing] or T2. With that sort of picture, I would have a discussion with the patient about potential treatment, with all of the various caveats.
Dr. Cree: Sure.
Dr. Freedman: So if I could sum up, general recommendations are very hard to make at this point without the evidence. There are cases that, discussed individually with an intelligent individual who has read [the literature] and is very anxious and knows the pros and cons of taking the medication, it might be reasonable to consider treatment in such individuals. But it is case by case until we have the evidence that treating RIS makes a difference in the long run. I think, gentlemen, you have put all the important facts on the table and certainly for you the viewers this is something that you will be facing in your practices. The decisions are not clear, but we look forward to new evidence and that evidence should help us deal with the RIS syndrome. Thank you for your attention today.
Red Sox prospect out of brain surgery rehab
Boston Red Sox minor league prospect Ryan Westmoreland has been released from a Boston rehabilitation hospital more than a month after brain surgery.
The team announced Tuesday that the 19-year-old outfielder was released on Saturday and will continue physical and occupational therapy as an outpatient at Spaulding Rehabilitation Hospital.
Westmoreland had surgery in March to remove a cavernous malformation in his brain.
A cavernous malformation is a cluster of abnormal or dilated blood vessels that affects the central nervous system. Symptoms can include bleeding in the brain, seizures and headaches.
The team says he has been making steady progress and is in great spirits.
The team announced Tuesday that the 19-year-old outfielder was released on Saturday and will continue physical and occupational therapy as an outpatient at Spaulding Rehabilitation Hospital.
Westmoreland had surgery in March to remove a cavernous malformation in his brain.
A cavernous malformation is a cluster of abnormal or dilated blood vessels that affects the central nervous system. Symptoms can include bleeding in the brain, seizures and headaches.
The team says he has been making steady progress and is in great spirits.
Uncontrolled brain activity linked to epilepsy
Researchers have shed new light on the mechanism behind epilepsy attacks in the brain, revealing a potential new target for drug treatment.
Around half a million people in the UK have some form of epilepsy.
Until recently the focus of research has been on cells called neurons, but a U.S. study points to a completely different cell.
Nature Neuroscience journal reports its behavior may be key to uncontrolled brain activity behind the condition.
Epilepsy attacks, which can manifest as fits in some people, or “absences” in others, are caused by too much electrical signaling from the brain's neurons.
However, in many cases, the reason for this over-activity is poorly understood.
Scientists now believe that, in some cases, although the problem happens at the neuron the underlying reason may be the failure of surrounding cells to help control this activity.
The latest study, from the Tuft University School of Medicine and the Children's Hospital of Philadelphia, provides the strongest evidence yet that a cell called an astrocyte is the culprit.
The astrocyte is known to have a wide range of functions, including supplying nutrients to other brain cells, and even helping the brain cope with damaged nerve cells.
In some brain diseases, the astrocytes swell up and behave differently, and it is this condition which the researchers believe is linked to epilepsy.
They induced this swelling in brain samples from mice, then tested whether this made a difference to the ability of the brain cells to “turn down”, or inhibit, the brain signals from specific neurons.
They found that the enlarged astrocytes led to reduced levels of a brain chemical known to inhibit electrical signalling from the neurons.
Dr. Douglas Coulter, one of the researchers, said: “We already know that inhibition is a powerful force in the brain.
“In epilepsy, inhibition is not working properly, and uncontrolled signaling leads to epileptic seizures.
“By better understanding the detailed events that occur in epilepsy, we are gaining knowledge that could ultimately lead to better treatments for epilepsy, and possibly for other neurological diseases.”
Professor Vincenzo Crunelli, a neuroscientist from the University of Cardiff, said other research, including his own, now pointed towards a role for astrocytes in various different types of epilepsy.
He said the finding might be particularly relevant in a form of epilepsy called temporal lobe epilepsy, which can be resistant to treatment.
He said: “This certainly suggests that the astrocytes may be involved in maintaining this over-excitation of the neurons.
“If this is the case, it offers the chance of a new therapeutic target.”
Around half a million people in the UK have some form of epilepsy.
Until recently the focus of research has been on cells called neurons, but a U.S. study points to a completely different cell.
Nature Neuroscience journal reports its behavior may be key to uncontrolled brain activity behind the condition.
Epilepsy attacks, which can manifest as fits in some people, or “absences” in others, are caused by too much electrical signaling from the brain's neurons.
However, in many cases, the reason for this over-activity is poorly understood.
Scientists now believe that, in some cases, although the problem happens at the neuron the underlying reason may be the failure of surrounding cells to help control this activity.
The latest study, from the Tuft University School of Medicine and the Children's Hospital of Philadelphia, provides the strongest evidence yet that a cell called an astrocyte is the culprit.
The astrocyte is known to have a wide range of functions, including supplying nutrients to other brain cells, and even helping the brain cope with damaged nerve cells.
In some brain diseases, the astrocytes swell up and behave differently, and it is this condition which the researchers believe is linked to epilepsy.
They induced this swelling in brain samples from mice, then tested whether this made a difference to the ability of the brain cells to “turn down”, or inhibit, the brain signals from specific neurons.
They found that the enlarged astrocytes led to reduced levels of a brain chemical known to inhibit electrical signalling from the neurons.
Dr. Douglas Coulter, one of the researchers, said: “We already know that inhibition is a powerful force in the brain.
“In epilepsy, inhibition is not working properly, and uncontrolled signaling leads to epileptic seizures.
“By better understanding the detailed events that occur in epilepsy, we are gaining knowledge that could ultimately lead to better treatments for epilepsy, and possibly for other neurological diseases.”
Professor Vincenzo Crunelli, a neuroscientist from the University of Cardiff, said other research, including his own, now pointed towards a role for astrocytes in various different types of epilepsy.
He said the finding might be particularly relevant in a form of epilepsy called temporal lobe epilepsy, which can be resistant to treatment.
He said: “This certainly suggests that the astrocytes may be involved in maintaining this over-excitation of the neurons.
“If this is the case, it offers the chance of a new therapeutic target.”
Brain Drain Review
April 27, 2010 - Brain Drain should have had a different name. Farm Swapper. Animal Spinner. Anything else. Because Brain Drain sounds kind of cool and fun, and this wimpy puzzler is anything but.
You're given a grid of animal-shaped icons in this one, and you've got to spin them around in groups of four at a time to make their positions match a pre-set goal that's displayed on the left side of the screen. So if the goal is to get four frogs on top and four ducks on the bottom, you'll move the cursor around and spin frogs and ducks until they line up that way. It's a bit like a Rubik's Cube -- you know the goal you're working for there, with each side displaying only one color. The game is just to spin the pre-set pieces the right way to get them to that end state.
It's a decent premise, but the presentation is a total mismatch -- the name, the animals, the music behind it all. Brain Drain feels like it was slapped together in about a week, and the diverse array of errors in grammar found in its Operations Guide lend further support to that theory. The gameplay stays too simple for too long, too -- some levels actually get less complicated as you move forward, instead of more difficult. You'll be able to solve several in, literally, less than five seconds. And the challenge-increasing tricks that do end up getting thrown at you, like pieces that turn invisible, are more annoying than they are challenging.
You're given a grid of animal-shaped icons in this one, and you've got to spin them around in groups of four at a time to make their positions match a pre-set goal that's displayed on the left side of the screen. So if the goal is to get four frogs on top and four ducks on the bottom, you'll move the cursor around and spin frogs and ducks until they line up that way. It's a bit like a Rubik's Cube -- you know the goal you're working for there, with each side displaying only one color. The game is just to spin the pre-set pieces the right way to get them to that end state.
It's a decent premise, but the presentation is a total mismatch -- the name, the animals, the music behind it all. Brain Drain feels like it was slapped together in about a week, and the diverse array of errors in grammar found in its Operations Guide lend further support to that theory. The gameplay stays too simple for too long, too -- some levels actually get less complicated as you move forward, instead of more difficult. You'll be able to solve several in, literally, less than five seconds. And the challenge-increasing tricks that do end up getting thrown at you, like pieces that turn invisible, are more annoying than they are challenging.
Mediterranean Diet May Save Brainpower
Study Shows a Benefit of Mediterranean Diet May Be Slower Mental Decline as People Age
April 27, 2010 (Anaheim, Calif.) -- Eat more like a Greek, and less like a typical American, and you may be doing your brain a favor, new research suggests.
Exactly why the diet, already known for its heart-healthy effects, may protect brain function isn't known, Tangney tells WebMD, but her research builds on other studies finding the diet preserves thinking and intellectual skills.
''I think there's a strong cardiovascular component," she says. Some of the diet components, such as the phytochemicals from fruits and vegetables, are thought to protect against neuron loss, she says.
The men and women answered a food-frequency questionnaire, spelling out in detail which components of the diet they ate and how often. The highest possible score for adherence to the Mediterranean diet is 55, but as Tangney notes, "No one followed it perfectly."
Tangney then classified their adherence to the diet as low, medium, or high. Low followers scored 12 to 25, medium 26 to 29, and high 30 to 45.
The researchers administered several tests of mental function, such as short- and long-term recall, and compiled those scores as a ''global cognitive score.'' The tests were given every three years.
Those in the top group knocked two years off their test scores, she says. For instance, if they were 65, they scored in the typical range for a 63-year-old.
There was some effect in the medium group, Tangney says, but no effect in the group that adhered the least.
The beauty of the finding, Tangney tells WebMD, is that following the diet perfectly isn't necessary to get a brain-protective effect. "When someone incorporates a diet rich in fruits and vegetables and non-refined grains such as cereals and breads and breaks it up with a little wine, there appears to be at least some protection against cognitive aging," she says.
While Tangney's team didn’t inquire about exercise habits, she says physical activity would be ideal to add to the Greek-like diet. "The true Mediterranean diet advocates lots of physical activity," she says.
Tangney says that's a plus of the study. Many studies have focused on individual nutrients and their effect on health.
But her research looks at the ''big picture" of the Mediterranean diet and finds benefits for those who follow it closely, but not perfectly.
Her advice? ''Eat lots of whole grains, legumes, and beans. Have an occasional glass of wine."
April 27, 2010 (Anaheim, Calif.) -- Eat more like a Greek, and less like a typical American, and you may be doing your brain a favor, new research suggests.
Older adults who adhere to the heart-healthy Mediterranean diet -- rich in fruits, vegetables, olive oil, legumes, fish, and moderate amounts of wine -- appear to have less mental decline with age, according to one of the latest studies on the health benefits of eating like a Greek.
''Those who adhered most closely to the Mediterranean diet performed as if they were two years younger," says study researcher Christy Tangney, PhD, a researcher at Rush University Medical Center, Chicago, who presented her findings Monday at EB 2010, the annual Experimental Biology meeting.Exactly why the diet, already known for its heart-healthy effects, may protect brain function isn't known, Tangney tells WebMD, but her research builds on other studies finding the diet preserves thinking and intellectual skills.
''I think there's a strong cardiovascular component," she says. Some of the diet components, such as the phytochemicals from fruits and vegetables, are thought to protect against neuron loss, she says.
Following the Mediterranean Diet
Tangney and her colleagues followed 3,790 men and women enrolled in the ongoing Chicago Health and Aging Project. The average age of the participants was 75, but all were over age 65. The follow-up averaged more than seven years.The men and women answered a food-frequency questionnaire, spelling out in detail which components of the diet they ate and how often. The highest possible score for adherence to the Mediterranean diet is 55, but as Tangney notes, "No one followed it perfectly."
Tangney then classified their adherence to the diet as low, medium, or high. Low followers scored 12 to 25, medium 26 to 29, and high 30 to 45.
The researchers administered several tests of mental function, such as short- and long-term recall, and compiled those scores as a ''global cognitive score.'' The tests were given every three years.
Those in the top group knocked two years off their test scores, she says. For instance, if they were 65, they scored in the typical range for a 63-year-old.
There was some effect in the medium group, Tangney says, but no effect in the group that adhered the least.
The beauty of the finding, Tangney tells WebMD, is that following the diet perfectly isn't necessary to get a brain-protective effect. "When someone incorporates a diet rich in fruits and vegetables and non-refined grains such as cereals and breads and breaks it up with a little wine, there appears to be at least some protection against cognitive aging," she says.
While Tangney's team didn’t inquire about exercise habits, she says physical activity would be ideal to add to the Greek-like diet. "The true Mediterranean diet advocates lots of physical activity," she says.
Second Opinion
The study results ''are significant in that it tells us something may be going on'' with the Greek-like diet and mental skills, says Bruce Semon, MD, PhD, a Milwaukee doctor who reviewed the study findings for WebMD.''It's a moderate effect," he says of the two-year improvement found in the study.
Because the researchers looked at the diet as a whole, he says, it's difficult to separate out which food or foods deserve credit for preserving brainpower.Tangney says that's a plus of the study. Many studies have focused on individual nutrients and their effect on health.
But her research looks at the ''big picture" of the Mediterranean diet and finds benefits for those who follow it closely, but not perfectly.
Her advice? ''Eat lots of whole grains, legumes, and beans. Have an occasional glass of wine."
Some pediatrc brain tumors may be worsened by immune gene expression
Aurora, Colo. —More than half of children diagnosed with ependymoma brain tumors will recur and die after standard treatment—surgery and radiation—what UCCC researcher Dr. Nicholas Foreman calls “one of the most significant problems in pediatric neuro-oncology.”
About one in 11 pediatric brain tumors are ependymomas, with about 200 new diagnoses of the disease in the United States each year. Brain tumors are the most common cause of childhood cancer death, according to the National Cancer Institute.“As we looked closely at the tumor cells, we realized this immune expression wasn’t a function of the tumor, but of the immune cells which, in some cases, were in large quantities in the tumor,” says Foreman. “It turned out to be the first demonstration in any brain tumor that the immune status of the individual at diagnosis is directly related to his or her chance of being cured.”
The researchers also found that certain aspects of the immune function could be blocking treatment’s effectiveness, which flies against common belief that all immune reactions to a tumor are positive. Activation of macrophages, a type of immune cell, could trigger release of antibodies that work counter to treatment. These antibodies might serve both as a marker for poor outcome and a treatment target, Foreman says.
“The immune system is more complex than people had realized,” he says. “Using this new grant, we hope to identify which parts of immune function is good for killing these brain tumors and which parts help keep them alive or help them grow.”
Foreman’s work is based on a human model of the immune system and outcomes. Most other experiments have been done in animal models, which might work differently than human systems.
In the long run, Foreman hopes the studies lead to a blood test that will tell doctors at diagnosis whether a child will have a good or poor outcome with standard treatment, and a method for manipulating patients’ immune system during standard treatment make it more effective.
The discovery was published in the Nov. 16, 2009, issue of the Journal of Immunology, by Foreman and colleagues from the SOM and Children’s Oncology Group, a national research group. The experiments were initially done using tumor tissue samples Foreman began collecting when he arrived in Denver in 1995, which was linked to a database that holds information about the patient’s treatment and outcome. The new studies will be done on tissue collected by centers across the country.
Foreman, director of pediatric neuro-oncology at The Children’s Hospital and professor of pediatrics at the University of Colorado School of Medicine (SOM), and colleagues last year identified the reason why half of the tumors recur. He has just been awarded a $1.2 million, four-year grant from the National Cancer Institute to dig deeper into the discovery that expression of certain genes linked with immune function predicted good outcomes.
About one in 11 pediatric brain tumors are ependymomas, with about 200 new diagnoses of the disease in the United States each year. Brain tumors are the most common cause of childhood cancer death, according to the National Cancer Institute.“As we looked closely at the tumor cells, we realized this immune expression wasn’t a function of the tumor, but of the immune cells which, in some cases, were in large quantities in the tumor,” says Foreman. “It turned out to be the first demonstration in any brain tumor that the immune status of the individual at diagnosis is directly related to his or her chance of being cured.”
The researchers also found that certain aspects of the immune function could be blocking treatment’s effectiveness, which flies against common belief that all immune reactions to a tumor are positive. Activation of macrophages, a type of immune cell, could trigger release of antibodies that work counter to treatment. These antibodies might serve both as a marker for poor outcome and a treatment target, Foreman says.
“The immune system is more complex than people had realized,” he says. “Using this new grant, we hope to identify which parts of immune function is good for killing these brain tumors and which parts help keep them alive or help them grow.”
Foreman’s work is based on a human model of the immune system and outcomes. Most other experiments have been done in animal models, which might work differently than human systems.
In the long run, Foreman hopes the studies lead to a blood test that will tell doctors at diagnosis whether a child will have a good or poor outcome with standard treatment, and a method for manipulating patients’ immune system during standard treatment make it more effective.
The discovery was published in the Nov. 16, 2009, issue of the Journal of Immunology, by Foreman and colleagues from the SOM and Children’s Oncology Group, a national research group. The experiments were initially done using tumor tissue samples Foreman began collecting when he arrived in Denver in 1995, which was linked to a database that holds information about the patient’s treatment and outcome. The new studies will be done on tissue collected by centers across the country.
Study: The human brain may not be special
CAMBRIDGE, England, April 27 (UPI) -- A British-led study has found striking similarities among the human brain, the nervous system of the nematode worm Caenorhabditis elegans and computer chips.
A team of U.K., U.S. and German neuroscientists and computer experts led by University of Cambridge Professor Edward Bullmore compared the way the systems are organized and found all three have the same networking principles.
The researchers said they found all three share two basic properties: All have the same architecture, with the same patterns repeating at different scales; and all show what's known as Rentian scaling -- a rule used to describe the relationship between the number of elements in a given area and the number of links between them.
"These striking similarities can probably be explained because they represent the most efficient way of wiring a complex network in a confined physical space -- be that a three-dimensional human brain or a two-dimensional computer chip," Bullmore said.
He said the findings, aside from expanding the understanding of the human brain's evolution, show humans can learn important lessons about evolution by studying the way in which technology has developed and by looking to very simple organisms such as the nematode.
"This challenges the commonly held belief that the human brain is special," Bullmore said. "In fact, it actually has much in common with simple organisms such as the worm and with other animal species."
A team of U.K., U.S. and German neuroscientists and computer experts led by University of Cambridge Professor Edward Bullmore compared the way the systems are organized and found all three have the same networking principles.
The researchers said they found all three share two basic properties: All have the same architecture, with the same patterns repeating at different scales; and all show what's known as Rentian scaling -- a rule used to describe the relationship between the number of elements in a given area and the number of links between them.
"These striking similarities can probably be explained because they represent the most efficient way of wiring a complex network in a confined physical space -- be that a three-dimensional human brain or a two-dimensional computer chip," Bullmore said.
He said the findings, aside from expanding the understanding of the human brain's evolution, show humans can learn important lessons about evolution by studying the way in which technology has developed and by looking to very simple organisms such as the nematode.
"This challenges the commonly held belief that the human brain is special," Bullmore said. "In fact, it actually has much in common with simple organisms such as the worm and with other animal species."
Study finds changes in astrocytes key to brain dysfunction
Modified cells disrupt signal control, may permit seizuresNeuroscience researchers have zeroed in on a novel mechanism that helps control the firing of electrical signals among neurons. By isolating the molecular and electrical events that occur when this control is disrupted, the new research sheds light on epileptic seizures and potentially on other prominent diseases involving poorly regulated brain activity.
"By better understanding the detailed events that occur in epilepsy, we are gaining knowledge that could ultimately lead to better treatments for epilepsy, and possibly for other neurological diseases," said neuroscientist Douglas A. Coulter, Ph.D., the corresponding author of the research study, from The Children's Hospital of Philadelphia. "Temporal lobe epilepsy, in particular, often resists current treatments."
Coulter's research group, collaborating with a team led by co-senior author Philip G. Haydon, Ph.D., of Tufts University School of Medicine, published a study online today in the journal Nature Neuroscience.
In epilepsy, excessive signaling between neurons, a major type of brain cell that communicates electrical signals across gaps called synapses, can lead to epileptic seizures. However, another class of brain cells called glia can regulate those signals. Among the glia are star-shaped cells called astrocytes-the particular focus of this research.
"This study shows that changes in astrocytes are key to brain dysfunction and opens the potential for novel therapeutic strategies in epilepsy," said Haydon, the Annetta and Gustav Grisard professor and chair of the department of neuroscience at Tufts.
The researchers focused on an abnormal condition called reactive astrocytosis, known to occur in many neurological diseases. The astrocytes swell to a large size and change expression levels of a number of proteins. The impact of reactive astrocytosis on brain function is difficult to investigate because it usually occurs in the context of brain inflammation and abnormal changes in surrounding cells.
The researchers solved this problem by using a virus to selectively cause reactive astrocytosis without triggering broader inflammation and brain injury, in a mouse model. They were able to focus on how the altered astrocytes affected specific synapses in neurons in the brain's hippocampus.
Studying the neuronal circuitry in brain slices from the mice, the study team found that changes in reactive astrocytes profoundly reduced the inhibitory control over brain signals.
Healthy brain function requires a delicate balance between excitation-the firing of brain signals-and inhibition, which limits those signals. An enzyme called glutamine synthetase is a key actor in a biological cycle that regulates the balance. The current study found that reactive astrocytosis reduces the supply of that enzyme, which in turn decreases inhibition and allows neurons to fire out of control.
"We already know that inhibition is a powerful force in the brain," said Coulter. "In epilepsy, inhibition is not working properly, and uncontrolled signaling leads to epileptic seizures. Because both disrupted inhibition and reactive astrocytosis are known to occur in other neurologic conditions, including many psychiatric disorders, traumatic brain injury, and neurodegenerative disorders such as Parkinson's disease, our findings may have wide implications."
Significantly, the researchers were able to dampen neuronal excitability in the animals' brain slices by adding glutamine, an amino acid that is depleted as a result of reduced glutamine synthetase activity. Coulter's and Haydon's teams are continuing animal studies to further investigate how this research may contribute to developing better treatments for epilepsy.
"By better understanding the detailed events that occur in epilepsy, we are gaining knowledge that could ultimately lead to better treatments for epilepsy, and possibly for other neurological diseases," said neuroscientist Douglas A. Coulter, Ph.D., the corresponding author of the research study, from The Children's Hospital of Philadelphia. "Temporal lobe epilepsy, in particular, often resists current treatments."
Coulter's research group, collaborating with a team led by co-senior author Philip G. Haydon, Ph.D., of Tufts University School of Medicine, published a study online today in the journal Nature Neuroscience.
In epilepsy, excessive signaling between neurons, a major type of brain cell that communicates electrical signals across gaps called synapses, can lead to epileptic seizures. However, another class of brain cells called glia can regulate those signals. Among the glia are star-shaped cells called astrocytes-the particular focus of this research.
"This study shows that changes in astrocytes are key to brain dysfunction and opens the potential for novel therapeutic strategies in epilepsy," said Haydon, the Annetta and Gustav Grisard professor and chair of the department of neuroscience at Tufts.
The researchers focused on an abnormal condition called reactive astrocytosis, known to occur in many neurological diseases. The astrocytes swell to a large size and change expression levels of a number of proteins. The impact of reactive astrocytosis on brain function is difficult to investigate because it usually occurs in the context of brain inflammation and abnormal changes in surrounding cells.
The researchers solved this problem by using a virus to selectively cause reactive astrocytosis without triggering broader inflammation and brain injury, in a mouse model. They were able to focus on how the altered astrocytes affected specific synapses in neurons in the brain's hippocampus.
Studying the neuronal circuitry in brain slices from the mice, the study team found that changes in reactive astrocytes profoundly reduced the inhibitory control over brain signals.
Healthy brain function requires a delicate balance between excitation-the firing of brain signals-and inhibition, which limits those signals. An enzyme called glutamine synthetase is a key actor in a biological cycle that regulates the balance. The current study found that reactive astrocytosis reduces the supply of that enzyme, which in turn decreases inhibition and allows neurons to fire out of control.
"We already know that inhibition is a powerful force in the brain," said Coulter. "In epilepsy, inhibition is not working properly, and uncontrolled signaling leads to epileptic seizures. Because both disrupted inhibition and reactive astrocytosis are known to occur in other neurologic conditions, including many psychiatric disorders, traumatic brain injury, and neurodegenerative disorders such as Parkinson's disease, our findings may have wide implications."
Significantly, the researchers were able to dampen neuronal excitability in the animals' brain slices by adding glutamine, an amino acid that is depleted as a result of reduced glutamine synthetase activity. Coulter's and Haydon's teams are continuing animal studies to further investigate how this research may contribute to developing better treatments for epilepsy.
Exercise your brain
It turns out that the old adage about how a healthy body leads to a healthy mind is being proven in the classroom

Brothers Theo, 11, and Loic Tremblay, 7, play street hockey close to their home in Outremont, last summer. Studies have shown that exercise just before tackling schoolwork can boost children's academic performance.
MONTREAL - Can't get your kids to concentrate on their homework? Don't nag. Send them out for a quick game of road hockey instead. Researchers report kids perform better academically after working up a sweat than after a day spent sitting around a classroom.
The idea that exercise and academic success go hand and hand is gaining more credibility. To the delight of physical education teachers everywhere, the message is filtering down to school administrators.
Naperville Central High School, located just outside Chicago, decided to see what would happen if they got some of their underperformers moving. Kids who scored poorly in math or reading went to the gym before sitting down to tackle a series of equations or read an assigned chapter of their text book.
The results were astounding. Kids who had previously struggled with school work improved their reading skills to the point where they were reading a year and a half above their grade level. Math scores rose by 21 per cent.
This small experiment jives with some of the latest research. Study ,after study reports not only that exercise has an immediate effect on test scores, but that fit kids do better in school than kids who don't exercise.
Physical activity, it seems, does more than just strengthen muscles; it strengthens the brain, too. Scientists suggest that kids who exercise on a regular basis solve problems faster than kids who don't. Fit kids are also more attentive and score higher when tested for accuracy.
The evidence is so strong that it's difficult to suggest that more time in study hall is the only answer to better grades. That being said, researchers are less clear about exactly how much exercise is needed to turn Cs into As. One of the first studies to try to pinpoint the exercise prescription necessary to stimulate learning was done in Trois Rivières and published in 1994. It stated that children who exercised an hour a day over and above their regular school gym class were more successful academically than students who got their exercise in gym class only.
Other studies suggest that only vigorous activity results in better academic performance, and some suggest that girls who exercise receive more scholastic benefit than active boys. As for how much exercise it takes to improve grades, the number varies from as low as 20 minutes a day to as high as 60 minutes. Also, elementary and middle school students are more suggestive to exercise interventions than high school students.
As for organized sport, that too has a positive effect on kids' report cards. A January 2010 article in the Journal of School Health reported that the grade-point averages for high school students who played on sports teams were higher than those who sat on the sidelines. It also reported that the more teams the students played on, the greater the boost to their GPA.
This wide spectrum of results is indicative of the complexity of collecting and evaluating exercise habits. Most people are generous when it comes to recounting the amount of time spent exercising. Then there's the difficulty of determining exercise intensity - what's moderate for some is easy for others.
There are less subjective ways to quantify physical activity. Pedometers and accelerometers measure daily activity, but are expensive, especially for large study samples.
That being said, there seems to be an agreement among researchers that not all exercise is equal in its ability to improve academic success. Aerobic exercise has proven more effective at boosting kids' test scores than muscular conditioning or stretching. And more exercise versus less produces more dramatic scholastic improvements.
Also interesting to note is that not all academic subjects reap the same benefits from exercise. Math scores seem to respond best to a bout of exercise compared with other subjects like English, history or geography.
Armed with the latest research, schools need to look at ways to incorporate more physical activity into the curriculum rather than less. Naperville High School went so far as to equip classrooms with stationary bikes and exercise balls, which allow students to exercise without leaving the classroom.
With that in mind, study hall may want to incorporate a little 4-on-4 soccer and math class should be scheduled right after gym class.
Parents should also rethink how their kids schedule homework. Take the family out for a bike ride or trip to the park before the kids hit the books after school. And participation in community or school-based sports should be encouraged and thought of as an academic asset, not a deterrent.
Keeping kids attentive and successful in school is the key to long-term academic success. And habits learned early are habits that tend to stick. So get out there with your kids and show them that exercise is not only the way to better health, it's also the way to better grades
The idea that exercise and academic success go hand and hand is gaining more credibility. To the delight of physical education teachers everywhere, the message is filtering down to school administrators.
Naperville Central High School, located just outside Chicago, decided to see what would happen if they got some of their underperformers moving. Kids who scored poorly in math or reading went to the gym before sitting down to tackle a series of equations or read an assigned chapter of their text book.
The results were astounding. Kids who had previously struggled with school work improved their reading skills to the point where they were reading a year and a half above their grade level. Math scores rose by 21 per cent.
This small experiment jives with some of the latest research. Study ,after study reports not only that exercise has an immediate effect on test scores, but that fit kids do better in school than kids who don't exercise.
Physical activity, it seems, does more than just strengthen muscles; it strengthens the brain, too. Scientists suggest that kids who exercise on a regular basis solve problems faster than kids who don't. Fit kids are also more attentive and score higher when tested for accuracy.
The evidence is so strong that it's difficult to suggest that more time in study hall is the only answer to better grades. That being said, researchers are less clear about exactly how much exercise is needed to turn Cs into As. One of the first studies to try to pinpoint the exercise prescription necessary to stimulate learning was done in Trois Rivières and published in 1994. It stated that children who exercised an hour a day over and above their regular school gym class were more successful academically than students who got their exercise in gym class only.
Other studies suggest that only vigorous activity results in better academic performance, and some suggest that girls who exercise receive more scholastic benefit than active boys. As for how much exercise it takes to improve grades, the number varies from as low as 20 minutes a day to as high as 60 minutes. Also, elementary and middle school students are more suggestive to exercise interventions than high school students.
As for organized sport, that too has a positive effect on kids' report cards. A January 2010 article in the Journal of School Health reported that the grade-point averages for high school students who played on sports teams were higher than those who sat on the sidelines. It also reported that the more teams the students played on, the greater the boost to their GPA.
This wide spectrum of results is indicative of the complexity of collecting and evaluating exercise habits. Most people are generous when it comes to recounting the amount of time spent exercising. Then there's the difficulty of determining exercise intensity - what's moderate for some is easy for others.
There are less subjective ways to quantify physical activity. Pedometers and accelerometers measure daily activity, but are expensive, especially for large study samples.
That being said, there seems to be an agreement among researchers that not all exercise is equal in its ability to improve academic success. Aerobic exercise has proven more effective at boosting kids' test scores than muscular conditioning or stretching. And more exercise versus less produces more dramatic scholastic improvements.
Also interesting to note is that not all academic subjects reap the same benefits from exercise. Math scores seem to respond best to a bout of exercise compared with other subjects like English, history or geography.
Armed with the latest research, schools need to look at ways to incorporate more physical activity into the curriculum rather than less. Naperville High School went so far as to equip classrooms with stationary bikes and exercise balls, which allow students to exercise without leaving the classroom.
With that in mind, study hall may want to incorporate a little 4-on-4 soccer and math class should be scheduled right after gym class.
Parents should also rethink how their kids schedule homework. Take the family out for a bike ride or trip to the park before the kids hit the books after school. And participation in community or school-based sports should be encouraged and thought of as an academic asset, not a deterrent.
Keeping kids attentive and successful in school is the key to long-term academic success. And habits learned early are habits that tend to stick. So get out there with your kids and show them that exercise is not only the way to better health, it's also the way to better grades
It's official: young drivers really do have underdeveloped brains
hare 
She said research has shown that inexperience, distractions from modern technology and a cultural tendency to "take risks" were the reason for most accidents.
"There is a biological element the prefrontal cortex of the brain is not fully developed until they are in their 20s," she said.
"This means their long-term planning skills, reasoning and impulse skills are all lacking.
"Typically, a lot of people might speed because they love the adrenaline rush it's sensation seeking.
"I guess you want to experience certain impulses and as we get older, you might have the same impulse but you will think of the consequences as well."
Drivers aged 16 to 24 account for 13 per cent of the state's drivers but were last year involved in 33 per cent of fatal crashes.
Dr Wundersitz, who will host a seminar today on young driver behaviour, said the most dangerous time for young drivers was during the first six months of their probationary license.
"That's thought to be because of two factors inexperience and risk-taking behaviour," she said.
"Risk-taking behaviour is particularly prevalent in young males.
Distractions
"This is a difficult issue because risk-taking is promoted in our culture it's everywhere, it's on television and it's looked at as being a highly prized virtue.
"But risky behaviour on our roads is not cool and it should not be seen as desirable."
Dr Wundersitz said modern technology was also leading to an increase in young driver crashes.
"You have mobile phones, GPS, iPods, entertainment screens it can be quite distracting.
"An inexperienced driver suddenly has to divide their attention between driving and these distractions.
"It's more difficult for them than a more experienced driver, where the driving process is more automated."
She said technological advances in cars would go a long way to keeping young drivers safe but newer vehicles were often used by parents.
"Electronic stability control detects a loss of steering control and automatically brakes individual wheels," Dr Wundersitz said.
"Lots of young people are involved in crashes that are just a single vehicle losing control.
"ESC has been found to have reduced single vehicle crashes by around 35 per cent. The problem is, young drivers usually drive vehicles that are on average 14 years old."
Dr Wundersitz said the Centre for Automotive Research wanted the State Government to restrict passenger numbers for inexperienced drivers to prevent them falling victim to pressure from their mates.
The Government has already passed legislation to extend the learner period from six to 12 months.
- Add to Digg
- Add to del.icio.us
- Add to Facebook
- Add to Kwoff
- Add to Myspace
- Add to Newsvine
- What are these?

Young drivers tend to be more impulsive for biological reasons. Picture: Calum Robertson / The Advertiser Source: The Advertiser
- Prefrontal cortex not fully developed
- Part of brain involved in reasoning
- Pressure on young males to take risks
YOUNG drivers have underdeveloped brains that make them more impulsive and less able to properly assess risks - reasons why they are involved in so many crashes.
Dr Lisa Wundersitz, from the Centre for Automotive Research, said brain development was one of three key issues behind the high number of young people injured or killed on our roads.She said research has shown that inexperience, distractions from modern technology and a cultural tendency to "take risks" were the reason for most accidents.
"There is a biological element the prefrontal cortex of the brain is not fully developed until they are in their 20s," she said.
"This means their long-term planning skills, reasoning and impulse skills are all lacking.
"Typically, a lot of people might speed because they love the adrenaline rush it's sensation seeking.
Drivers aged 16 to 24 account for 13 per cent of the state's drivers but were last year involved in 33 per cent of fatal crashes.
Dr Wundersitz, who will host a seminar today on young driver behaviour, said the most dangerous time for young drivers was during the first six months of their probationary license.
"That's thought to be because of two factors inexperience and risk-taking behaviour," she said.
"Risk-taking behaviour is particularly prevalent in young males.
Distractions
"This is a difficult issue because risk-taking is promoted in our culture it's everywhere, it's on television and it's looked at as being a highly prized virtue.
"But risky behaviour on our roads is not cool and it should not be seen as desirable."
Dr Wundersitz said modern technology was also leading to an increase in young driver crashes.
"You have mobile phones, GPS, iPods, entertainment screens it can be quite distracting.
"An inexperienced driver suddenly has to divide their attention between driving and these distractions.
"It's more difficult for them than a more experienced driver, where the driving process is more automated."
She said technological advances in cars would go a long way to keeping young drivers safe but newer vehicles were often used by parents.
"Electronic stability control detects a loss of steering control and automatically brakes individual wheels," Dr Wundersitz said.
"Lots of young people are involved in crashes that are just a single vehicle losing control.
"ESC has been found to have reduced single vehicle crashes by around 35 per cent. The problem is, young drivers usually drive vehicles that are on average 14 years old."
Dr Wundersitz said the Centre for Automotive Research wanted the State Government to restrict passenger numbers for inexperienced drivers to prevent them falling victim to pressure from their mates.
The Government has already passed legislation to extend the learner period from six to 12 months.
Brain’s to raise a glass to £100m-plus turnover
FAMILY-OWNED brewing and hospitality company SA Brain & Co will reveal its latest end-of-year accounts in tomorrow’s Western Mail business supplement.
The figures will show that the business with headquarters in Cardiff delivered another £100m- plus turnover.
And despite continuing challenges from the downturn, it is also on course to increase profits in its current financial year to the end of September, 2010.
Chief executive of the company – which has 260 managed pubs – Scott Waddington will also outline that longer-term the company plans to make further acquisitions.
The publication will also feature an in-depth analysis of corporate deals in Wales over the last decade, complied by Cardiff-based corporate finance advisory firm Gambit.
The figures will show that the business with headquarters in Cardiff delivered another £100m- plus turnover.
And despite continuing challenges from the downturn, it is also on course to increase profits in its current financial year to the end of September, 2010.
Chief executive of the company – which has 260 managed pubs – Scott Waddington will also outline that longer-term the company plans to make further acquisitions.
The publication will also feature an in-depth analysis of corporate deals in Wales over the last decade, complied by Cardiff-based corporate finance advisory firm Gambit.
Uncontrolled brain activity linked to epilepsy

The Hindu Model of the brain. Photo: The Hindu Archives
An American study has shed new light on the mechanism behind epilepsy attacks in the brain.
Neuroscientist Douglas A. Coulter, the co-author of the research study, from The Children’s Hospital of Philadelphia, said: “By better understanding the detailed events that occur in epilepsy, we are gaining knowledge that could ultimately lead to better treatments for epilepsy, and possibly for other neurological diseases.
“Temporal lobe epilepsy, in particular, often resists current treatments.” For the research, Coulter and colleagues, collaborated with a team led by co-senior author Philip G. Haydon, of Tufts University School of Medicine.
In epilepsy, excessive signalling between neurons, a major type of brain cell that communicates electrical signals across gaps called synapses, can lead to epileptic seizures. However, another class of brain cells called glia can regulate those signals. Among the glia are star-shaped cells called astrocytes-the particular focus of this research.
Haydon, the Annetta and Gustav Grisard professor and chair of the department of neuroscience at Tufts, said: “This study shows that changes in astrocytes are key to brain dysfunction and opens the potential for novel therapeutic strategies in epilepsy. The researchers focused on an abnormal condition called reactive astrocytosis, known to occur in many neurological diseases. The astrocytes swell to a large size and change expression levels of a number of proteins. The impact of reactive astrocytosis on brain function is difficult to investigate because it usually occurs in the context of brain inflammation and abnormal changes in surrounding cells.
The researchers solved this problem by using a virus to selectively cause reactive astrocytosis without triggering broader inflammation and brain injury, in a mouse model. They were able to focus on how the altered astrocytes affected specific synapses in neurons in the brain’s hippocampus.
Studying the neuronal circuitry in brain slices from the mice, the study team found that changes in reactive astrocytes profoundly reduced the inhibitory control over brain signals. Healthy brain function requires a delicate balance between excitation -- the firing of brain signals -- and inhibition, which limits those signals. An enzyme called glutamine synthetase is a key actor in a biological cycle that regulates the balance. The current study found that reactive astrocytosis reduces the supply of that enzyme, which in turn decreases inhibition and allows neurons to fire out of control. Coulter said: “We already know that inhibition is a powerful force in the brain.
“In epilepsy, inhibition is not working properly, and uncontrolled signalling leads to epileptic seizures. Because both disrupted inhibition and reactive astrocytosis are known to occur in other neurologic conditions, including many psychiatric disorders, traumatic brain injury, and neurodegenerative disorders such as Parkinson’s disease, our findings may have wide implications.” Significantly, the researchers were able to dampen neuronal excitability in the animals’ brain slices by adding glutamine, an amino acid that is depleted as a result of reduced glutamine synthetase activity. The study has appeared in the journal Nature Neuroscience.
Subscribe to:
Comments (Atom)




