Cancer claimed the life of medical marijuana poster child Cash “Cashy”
Hyde after access to cannabis-based medication was cut off by a sweeping
medical marijuana crackdown in Montana last summer
MISSOULA, MT — Cash “Cashy” Hyde passed away in his father’s arms this week. The four-year-old Montana boy—whose malignant brain cancer had been in remission while he received consistent medical cannabis treatments—is the latest casualty in the federal government’s war on voter-approved medical marijuana, says John Malanca, a close friend of the Hyde family.
 Malanca recounts the Hyde family’s ordeal:
Malanca recounts the Hyde family’s ordeal:
Desperate to find anything to keep their young child Cash alive, after traditional treatments and medications failed to slow the growth of the malignant tumor in his brain, Mike and Kalli Hyde turned to high-CBD cannabis oil. Cash’s cancer immediately went into remission, and he started to live a more normal life.
Cash was comfortable, started eating again, and recovered his desire to play.
Then, last summer, law enforcement officials in Montana came down hard on the medical marijuana industry.
Rather than face the risk of being stormed by armed agents and subjected to steep fines or jail time, many legally-compliant medical cannabis dispensaries in Montana closed down.
The federal crackdown resulted in the closure of most of the medical marijuana dispensaries in Montana, and cut off the Hyde’s access to the therapeutic cannabis oil that was keeping Cash’s cancer at bay. Once Cash’s medication was cut off, his cancer came back out of remission.
“We put out a call to action, asking people to donate cannabis oil for Cash’s health—and there was a heart-warming outpouring of donors and support,” said Malanca. “Unfortunately, by the time we got Cash the medication he needed, his cancer could no longer be controlled.”
The Hyde Family has established the Cash Hyde Foundation to help prevent unnecessary loss of health and life through advocacy of progressive and responsible medical marijuana policies, law enforcement, and legislation: “Cashy’s Law.”
The foundation also supports increased medical marijuana research, cannabis health education, and pediatric cancer research.
“Cannabis oil extended Cash’s life; he beat cancer twice,” said Malanca. “He brought so much love to this world and so many people together. He educated people.”
MISSOULA, MT — Cash “Cashy” Hyde passed away in his father’s arms this week. The four-year-old Montana boy—whose malignant brain cancer had been in remission while he received consistent medical cannabis treatments—is the latest casualty in the federal government’s war on voter-approved medical marijuana, says John Malanca, a close friend of the Hyde family.
 Malanca recounts the Hyde family’s ordeal:
Malanca recounts the Hyde family’s ordeal:Desperate to find anything to keep their young child Cash alive, after traditional treatments and medications failed to slow the growth of the malignant tumor in his brain, Mike and Kalli Hyde turned to high-CBD cannabis oil. Cash’s cancer immediately went into remission, and he started to live a more normal life.
Cash was comfortable, started eating again, and recovered his desire to play.
Then, last summer, law enforcement officials in Montana came down hard on the medical marijuana industry.
Rather than face the risk of being stormed by armed agents and subjected to steep fines or jail time, many legally-compliant medical cannabis dispensaries in Montana closed down.
The federal crackdown resulted in the closure of most of the medical marijuana dispensaries in Montana, and cut off the Hyde’s access to the therapeutic cannabis oil that was keeping Cash’s cancer at bay. Once Cash’s medication was cut off, his cancer came back out of remission.
“We put out a call to action, asking people to donate cannabis oil for Cash’s health—and there was a heart-warming outpouring of donors and support,” said Malanca. “Unfortunately, by the time we got Cash the medication he needed, his cancer could no longer be controlled.”
The Hyde Family has established the Cash Hyde Foundation to help prevent unnecessary loss of health and life through advocacy of progressive and responsible medical marijuana policies, law enforcement, and legislation: “Cashy’s Law.”
The foundation also supports increased medical marijuana research, cannabis health education, and pediatric cancer research.
“Cannabis oil extended Cash’s life; he beat cancer twice,” said Malanca. “He brought so much love to this world and so many people together. He educated people.”


 Washington:
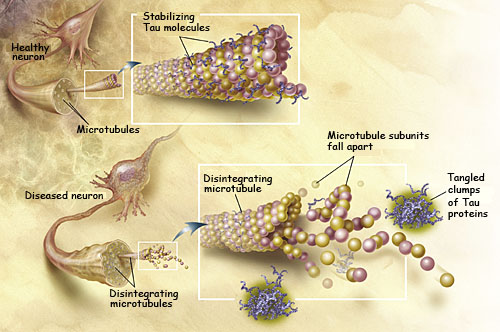
Researchers have developed a molecular compound CLR01 dubbed “molecular
tweezers,” which prevents toxic proteins from aggregating or clumping
together and killing brain cells in Alzheimer’s disease.
Washington:
Researchers have developed a molecular compound CLR01 dubbed “molecular
tweezers,” which prevents toxic proteins from aggregating or clumping
together and killing brain cells in Alzheimer’s disease.